Professor Tony Culyer
CURRICULUM
VITAE
Professor
Anthony John (Tony) Culyer, CBE, BA, Hon DEcon, Hon
FRCP, FRSA, FMedSci
|

|
Welcome to my Home
Page!
I hope that clicking on the appropriate topic below will get
you to where you want to be
If you have difficulty downloading anything, let me know and
Ill e-mail it to you
|
 CV
CV
 Current articles
Current articles
 Journal
of Health Economics
Journal
of Health Economics
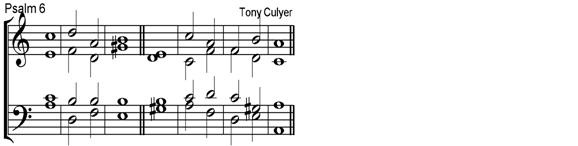
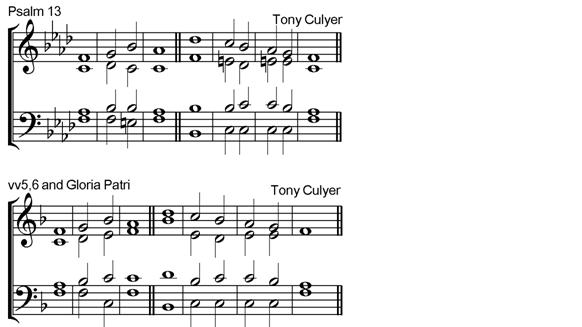
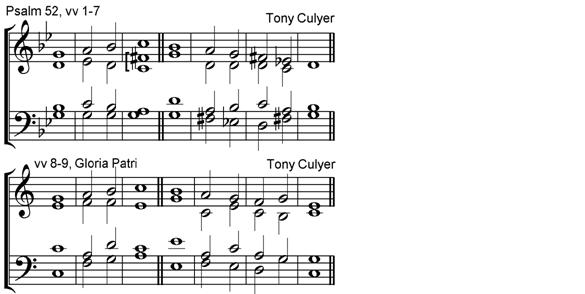
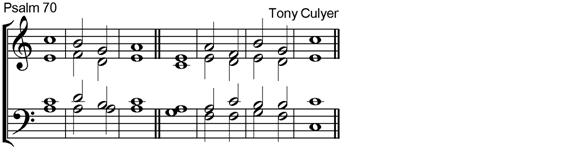
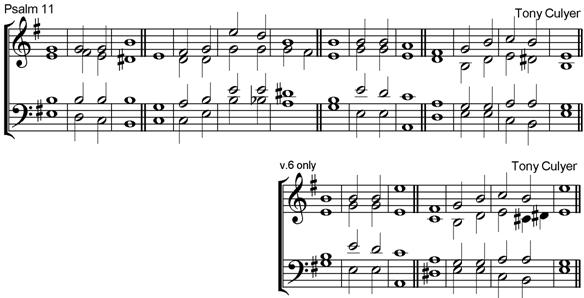
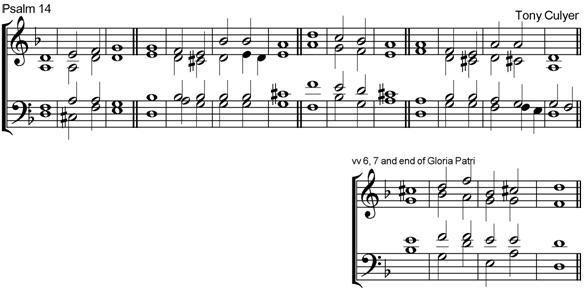
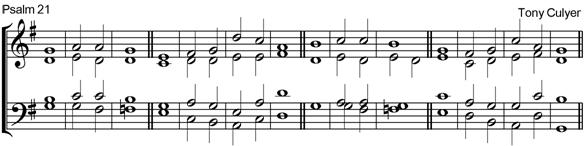
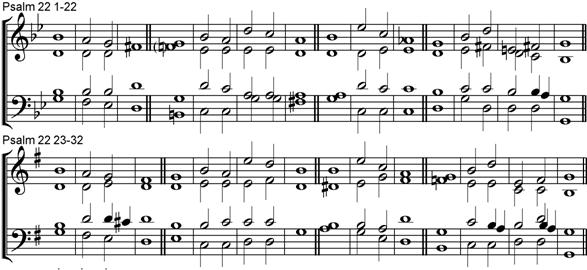
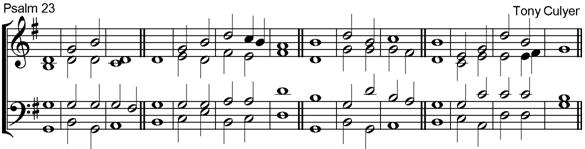
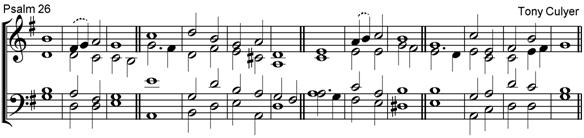
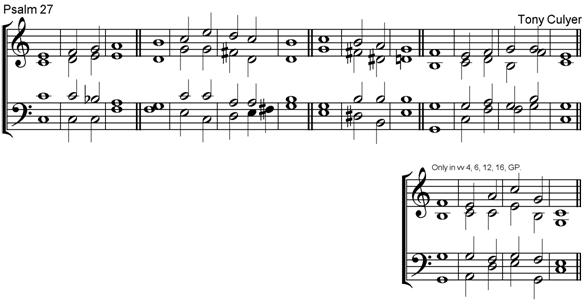
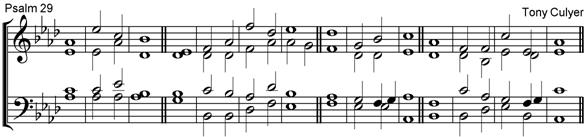
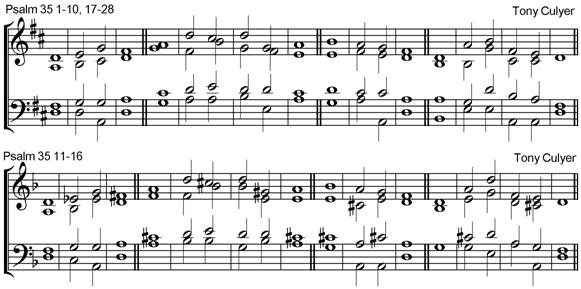
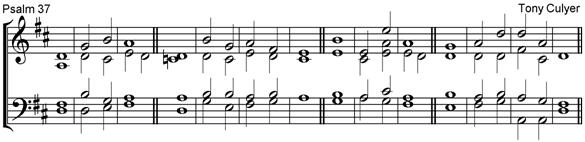
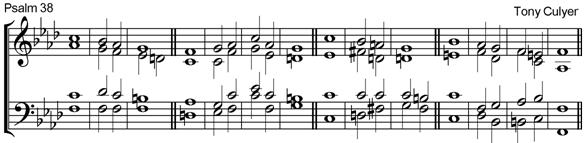
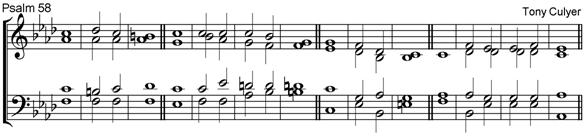
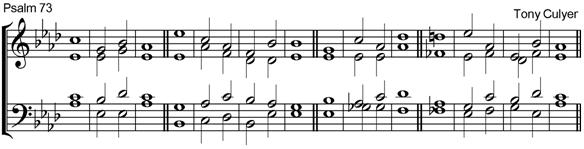
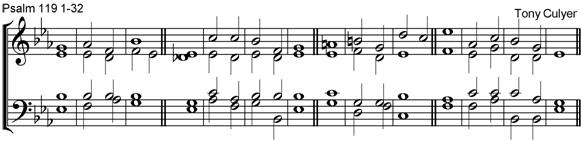
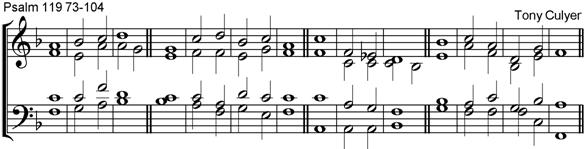
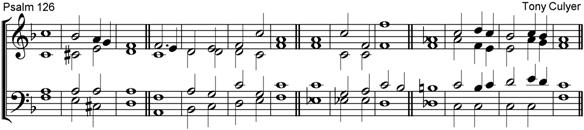
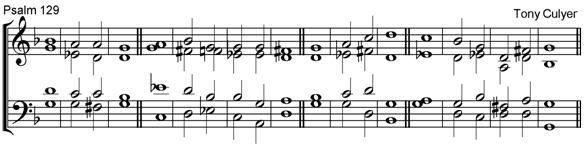
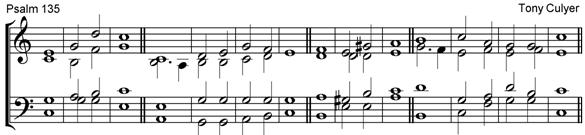
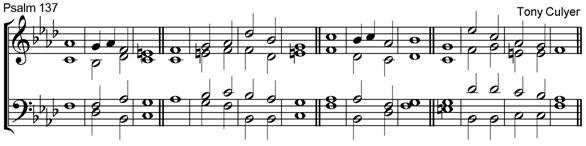
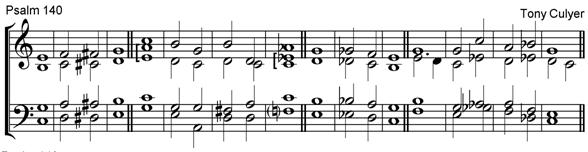
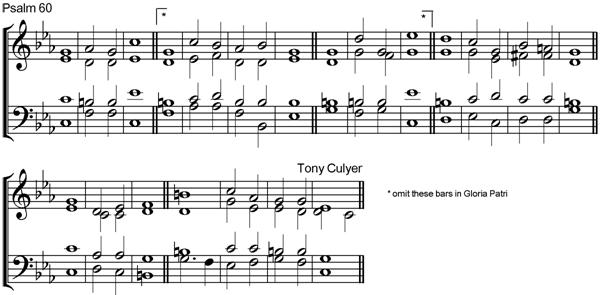
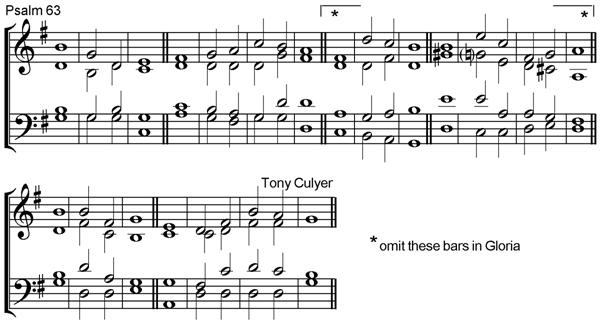
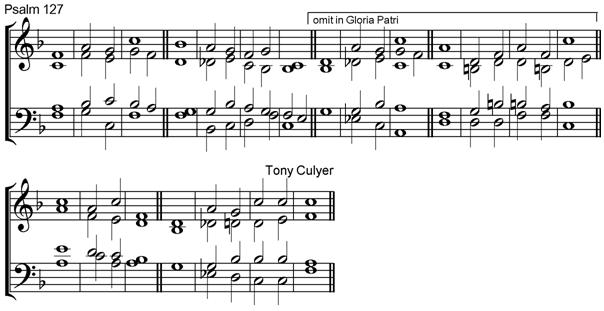
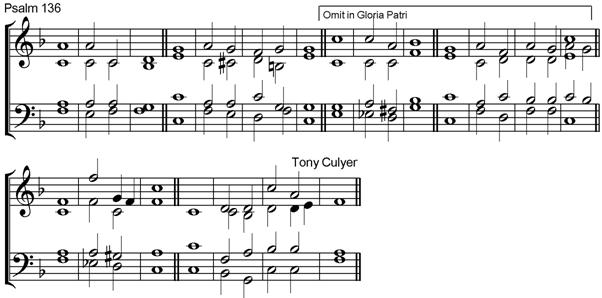
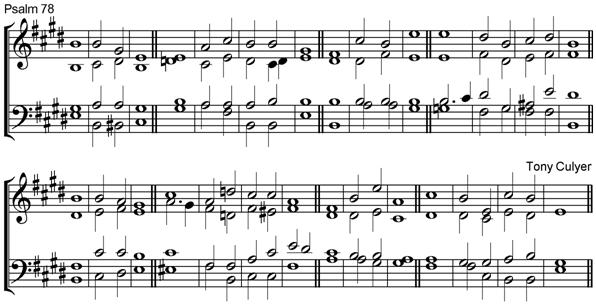
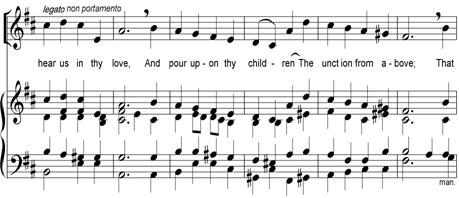
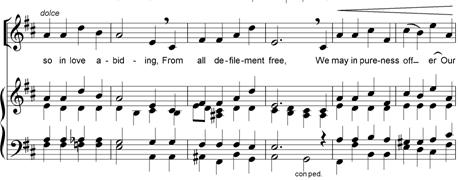
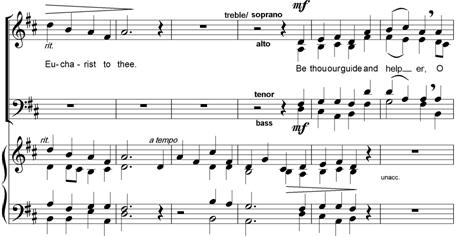
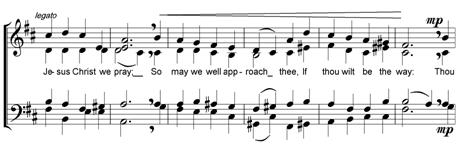
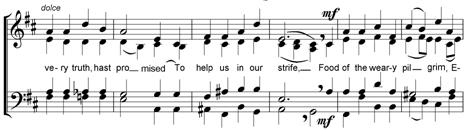
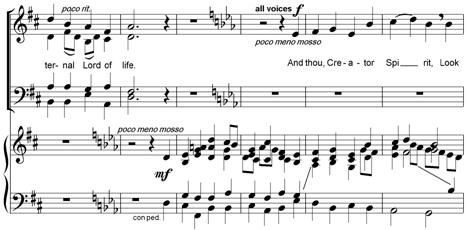
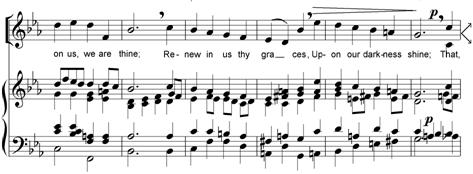
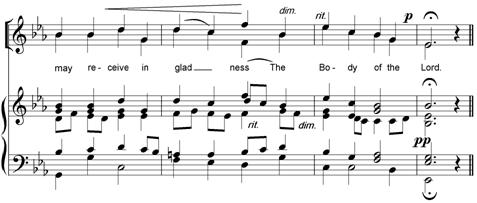
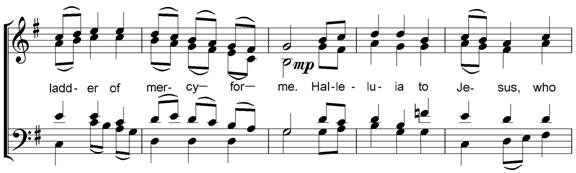
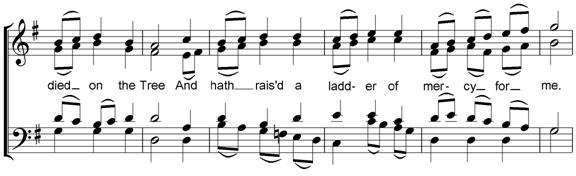
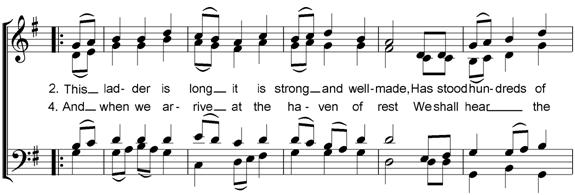
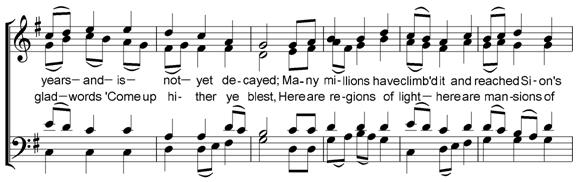
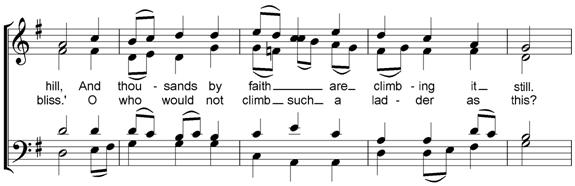
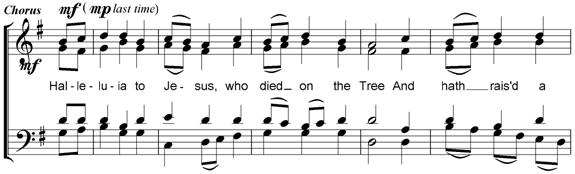
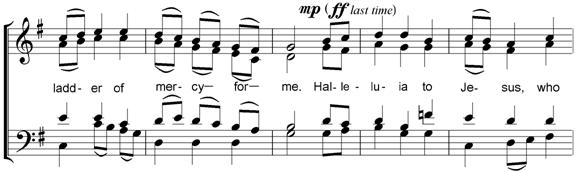
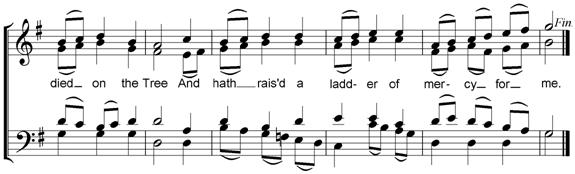
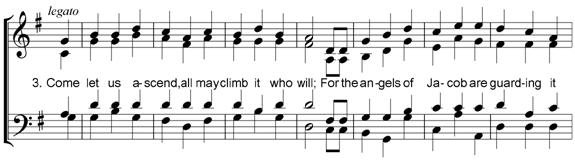
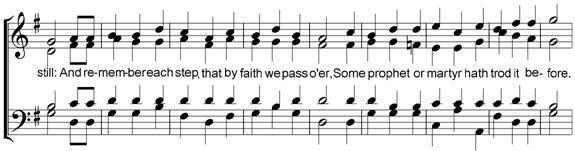
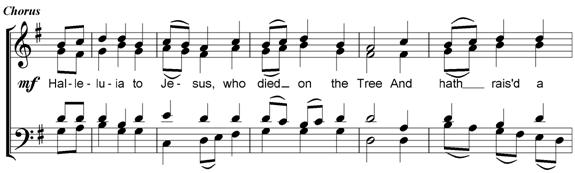
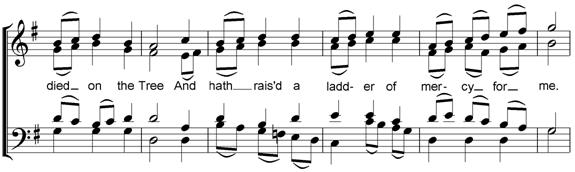
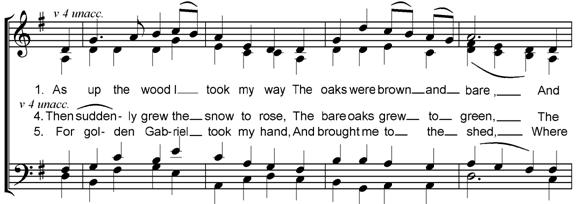
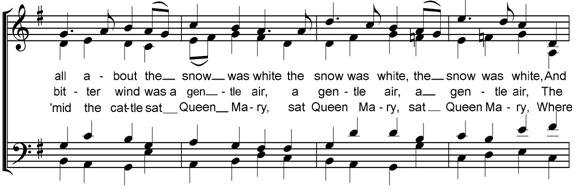
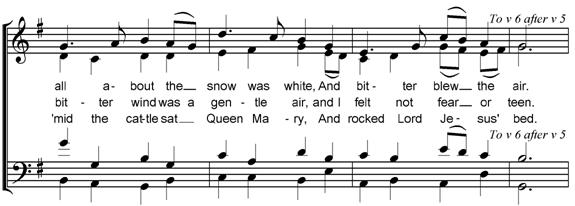
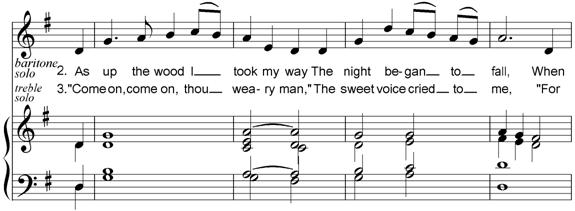
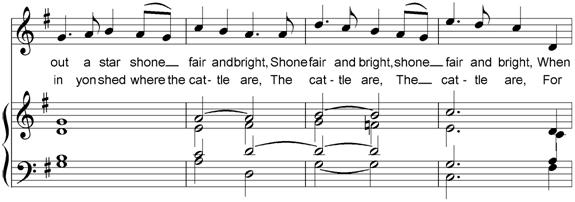
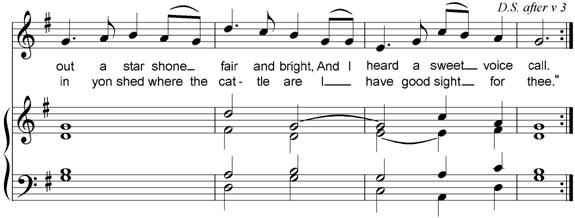
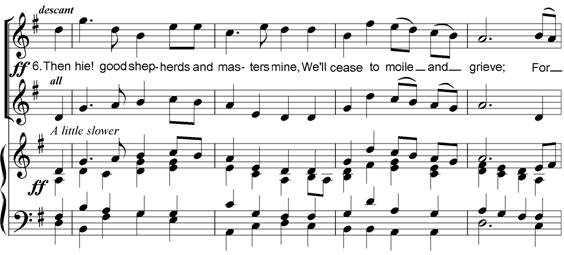
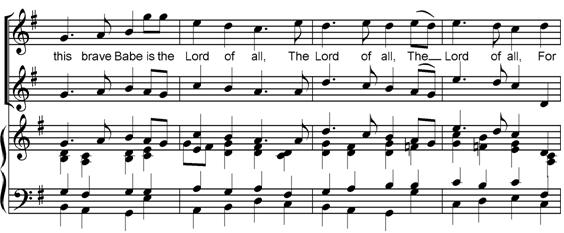
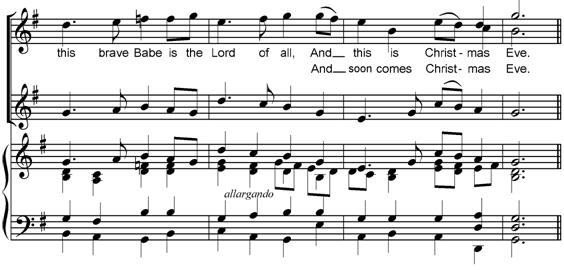
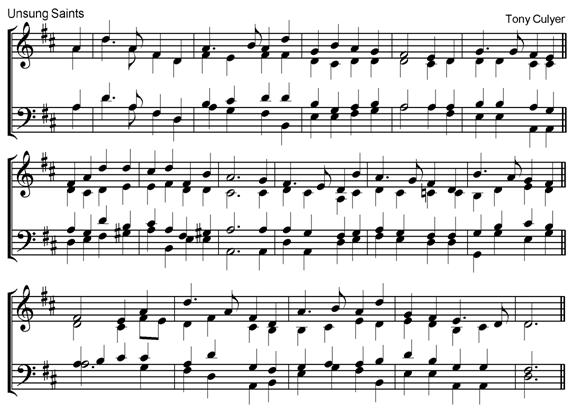
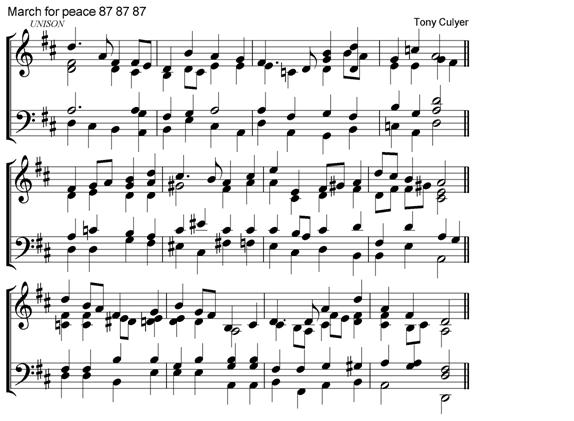
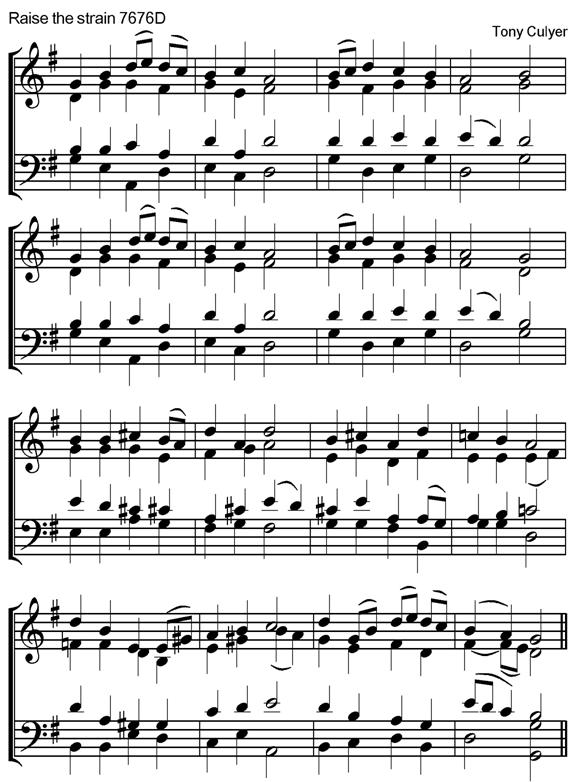
 Anglican Chants
Anglican Chants
 Other
Pieces
Other
Pieces
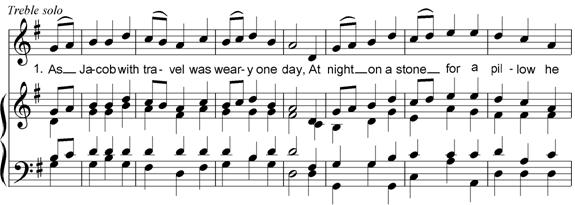
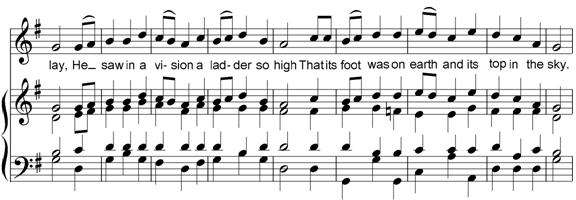
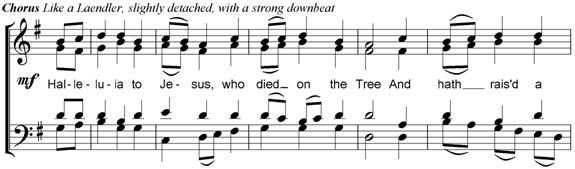
 Hymn
Tunes
Hymn
Tunes
 Royal
School of Church Music
Royal
School of Church Music
last update: November
2011
Personal background
Present Status
Ontario Research Chair in Health Policy & System Design, University of Toronto
Professor
of Economics, University of York,
England
Adjunct Scientist, Institute for Work and Health, Toronto
Chair,
WSIB Research Advisory Council (to March 2010)
Founding Co-Editor, Journal of Health Economics
Date of Birth
1 July 1942
Addresses
(Home, England): "The Laurels", Main Street, Barmby
Moor, York, Y042 4EJ, UK
Tel.
(0)1759-307177
E-mail: tonyandsiegi@btinternet.com
(Home, Canada):
80 Front Street East Suite 804,
Toronto, Ontario,
M5E 1T4, Canada
Tel: 416
369-9973
E-mail: tonyandsiegi@sympatico.ca
(University,
Canada): Department of Health Policy, Management and Evaluation, University of
Toronto, Faculty of Medicine, University of Toronto, Health Sciences
Building, 155 College Street, Suite 425, Toronto, Ontario M5T 3M6
Tel: 416
978 7340
Fax: 416-978-7350
E-mail: tony.culyer@utoronto.ca
(University, England):
Department of Economics & Related Studies, University
of York, Heslington,
York Y010 5DD, England
Tel: (0)1904-321420
Fax:
(0)1904-433759
E-mail: ajc17@york.ac.uk
Web page: http://www-users.york.ac.uk/~ajc17
Marital Status
Married from 1966 to 2011 to same partner Siegi, with son and daughter,
four grandchildren. Now widowed.
Secondary Education
Sir
William Borlase's School, Marlow
The King's
School, Worcester
University Education
Graduated
Exeter University
in 1964 (2(i)) in Economics, Exeter University
Leo T.
Little Prize for best graduating student in Economics 1964.
1964-5
Graduate Student and Teaching Assistant at the University of California
at Los
Angeles (plus Fulbright Travel Scholarship).
Degrees
B.A. (Hons), (Exeter)
(1964)
Doctor of
Economics, honoris causa
(Stockholm School of Economics) (1999)
Honours
Founding
Fellow of the Academy
of Medical Sciences
(1998)
Commander
of the British Empire (CBE) (1999)
Fellow of
the Royal Society of Arts (1999)
Doctor of
Economics, honoris causa
(Stockholm School of Economics) (1999)
Honorary
Fellow of the Royal College of Physicians of London (2003)
Fellowships of Academies
Founding Fellow
of the Academy of
Medical Sciences (1998)
Fellow of
the Royal Society of Arts (1999)
Honorary
Fellow of the Royal College of Physicians of London (2003)
University Career
1964-65 Teaching Assistant, University of California
at Los Angeles
1965-66 Tutor in Economics, University of Exeter
1966-69 Assistant Lecturer in Economics,
University of Exeter.
1969-72 Lecturer in Economics, University of York
1971-79 Assistant
Director, Institute of Social & Economic Research, University of York
1972-76 Senior Lecturer in Economics,
University of York
1976-79 Reader in Economics, University of York
1976 Senior Research Associate at the
Ontario
Economic Council
Visiting Professorial Lecturer at Queen's
University, Kingston, Canada
1979 William
Evans Visiting Professor, University
of Otago, Dunedin, New
Zealand
Visiting Fellow, Australian
National University,
Canberra, Australia
1979-82 Deputy
Director, Institute of Social and Economic Research, University of York
1979- Professor
of Economics, University
of York (since 1982 in
Department of Economics & Related Studies)
1983-84 Director of the Graduate Health Economics Programme,
Department of Economics & Related Studies, University of York
1985-86 Visiting Professor, Trent University,
Canada
1986-01 Head of Department of Economics &
Related Studies, University
of York
1989-94 Visiting
professor, Department of Health Administration, University of Toronto
1990-91 (Oct-Feb)
Visiting Professor, Institut für Medizinische Informatik und Systemforschung
(Gesellschaft für Strahlen-und Umweltforschung), Munich, Germany
1991
(Apr-Sep) Visiting
Professor, Department of Health Administration, University of Toronto
1991-94 Pro-Vice-Chancellor, University of York, England
1994-97 Deputy Vice-Chancellor, University of York, England
1995-96 Director, School
of Politics, Economics &
Philosophy, University
of York
1996
(November) Visiting
Professor, Central Institute of Technology,
New Zealand
1997-01 Director of Health Development, University of York
1999-01 Director (Board Member) of York Health Economics
Consortium
2001-03 Chair, Board of York Health Economics Consortium
2003-07 Visiting
Professor, Department of Health Policy, Management & Evaluation, University
of Toronto
2003-06 Chief
Scientist, Institute for Work &
Health, Canada
2006-07 Senior
Scientist, Institute for Work &
Health, Canada
2006-07 Senior
Economic Adviser, Cancer Care Ontario
2006-10 Chair,
Research Advisory Council of the Workplace Safety & Insurance Board
(Ontario)
2007- Ontario Research Chair in Health Policy and System
Design, University
of Toronto
2007- Adjunct
Scientist, Institute for Work & Health, Toronto
Affiliations
Academy
of Medical Sciences, Health Economists' Study Group, International Health
Economics Association, Royal Economic Society, Royal Society of Arts, Royal
College of Physicians (London), Royal School of Church Music, Royal School of
Church Music (Canada).
Journal Editing
1996-70 Acting
Editor, Assistant Editor, Editorial Board member
(various times), Social and Economic
Administration.
1982- Founding Co-editor, Journal of Health Economics
1984-85 Founding Editor, Nuffield/York Portfolios
1986-96 Advisory Editor, Social Science and Medicine
1976-84 Member, Editorial Board, Bulletin of Economic Research
1983-93 Founding Member, Editorial Panel, The Economic Review
1992-2002 Member, Editorial Board, Medical Law International
1994-2001 Member, Managing Committee, Journal of Medical Ethics
1995-2000 Member, Editorial Board, British Medical Journal
1996-2007 Founding
Member, International Advisory Board, Clinical
Effectiveness in Nursing
1998-2001 Member,
Editorial Advisory Board, Handbook on
Research Methods for Evidence Based Health Care
1999-2005 Member,
Editorial Board, Zeitschrift für die
gesamte Versicherungswissenschaft
2001 Guest Editor, Journal of Medical Ethics (Vol. 27, No.
4).
2009- Editor in Chief, The Elsevier on-line Encyclopedia of Health Economics,
External Academic Advisory
Boards
1989-92 Member,
Methodological Advisory Group on Non-economic Loss, Ontario Workers'
Compensation Board
1992-98 Member,
Advisory Committee of the Canadian Institute for Advanced Research (Population
Health Program)
1992-2001 Member,
Advisory Committee for Centre for Health and Society, University College,
London
1990-94 Member,
Research Advisory Committee of the Institute for Work and Health (Toronto,
Canada)
1997-2002 Member,
Research Advisory Committee of Canadian Institute for Health and Work
1997-2003 Member,
Research Advisory Committee of the Institute for Work and Health (Toronto,
Canada)
2000-03 Trustee, The
Canadian Health Services Research Foundation, Ottawa
2001 Member,
International Scientific Advisory Committee, Unit of Health Economics and
Technology Assessment in Health Care, Budapest University of Economics
2006-10 Member, International Advisory Board,
Alberta Bone & Joint Institute
2006-10 Chair,
Research Advisory Council, Workplace Safety and Insurance Board (Ontario)
2006-10 Member,
Advisory Board, Centre for Research Expertise in Musculo-Skeletal
Diseases, University of Waterloo
2006-10 Member,
Advisory Board, Centre for Research Expertise in Occupational Disease,
University of Toronto
2006-10 Member,
Advisory Board, Centre for Research Expertise in Improved Disability Outcomes,
University Health Network, Toronto
Professional Groups
1970-86 Founding Organiser,
Health Economists' Study Group (HESG)
1970- Member, HESG
1975-76, Member,
Scientific Committee of the International Institute of Public Finance
1975-90 Honorary Adviser
to the Office of Health Economics
1977-85 Member,
Organising Committee of International Seminar in
Public Economics
1979-85 Founding Course Coordinator for the Health Economics
option, Corporate Management Programme of King's Fund College, London
1980-82 Convenor, SSRC European Workshop in Health Indicators (for
report, see publications)
1982-83 Member,
Scientific Committee of the International Institute of Public Finance
1983-84 Director,
York MSc. Programme in Health Economics
1987-88 Member, Institute of Health Service Management Working
Party on Alternative Funding and Delivery of Health Services (for reports see
publications).
1987-2001 Member,
Conference of Heads of University Departments of Economics (CHUDE)
1988-93 Member, Standing Committee of CHUDE
1989-92 Member, College Committee of the
King's Fund College, London,
1990-97 Member
of Editorial Policy Committee, Office of Health Economics
1990-97 Member, Editorial Board, Office of
Health Economics
1991-93 Member,
Economics Association National Development Group on economics curriculum
development
1991-92 Council member,
Royal Economic Society
1992 World
Health Organisation Adviser (economics of schistosomiasis control in Kenya)
1992 Member,
Canadian Institute of Advanced Research (Review Panel on Population Health)
1992-97 Member,
Kenneth J. Arrow Award in Health Economics (Prize Committee)
1992-92 Member,
Institute of Health Services Management's "Future Health Care
Options" Working Party
1994 President, Section F (Economics),
British Association
1996 Member, ESRC Training Board Economics Area Panel
1996-2003 Member, Academic Advisory Council,
University of Buckingham
1997 Member
of World Health Organisation two-person mission to
Kazakhstan on the privatisation and reform of health
care services, February
1997-2001 Vice Chair, Office of Health Economics
1997- Chair, Office of Health Economics
Editorial Board
1988-93 Member, Standing Committee of CHUDE
2001- Chair, Office of Health Economics
Policy Board
2002-07 Member, Governing Board,
International Health Economics Association
2004- Chair, Office of Health Economics
Management Committee
2004-06 Adviser, Canada Health Council
2005 Member, Ontario Health
Technology Advisory Committee
2006-07 Senior Economic Advisor, Cancer Care
Ontario
2006-07 Economic Advisor, Ontario Ministry of
Health and Long Term Care
2006 Member,
Ontario Ministry of Health and Long Term Care Equity Editorial Board
2006-08 Canadian
Institutes for Health Research Michael Smith Prize in Health Research Committee
2007- Member,
Ontario Ministry of Health and Long Term Care Career Scientist Relevance Review
Panel
2007- Member,
Ontario Ministry of Health and
Long Term Care Health Research Advisory Council
2009- Member,
Hall Foundation Board (Canada)
2009- Member
Advisory Committee, NICE International
2009- Member,
Department of Health Policy Research Units Commissioning Panel
2009- Member,
Ontario Ministry of Health and Long Term Care, Health System Strategy Division,
External Advisory Group
2009- Member,
Ontario Ministry of Health and Long Term Care Advisory Group on Productivity
2009- Member,
Ontario Ministry of Health and Long Term Care Steering Committee for
Partnerships for Health System Improvement (CIHR project)
2010- 11 Member, Ontario
Health Quality Council Advisory Committee
Principal Lectures
1976 Plenary Lecture, First Canadian
Health Economics Symposium, Kingston
1980 Plenary
Lecture, First Australian Conference of Health Economists, Canberra
1986 Woodward Lecturer, University of
British Columbia
1986 Plenary
Lecture, Third Canadian Conference on Health Economics, Winnipeg
1990 Perey
Lecturer, McMaster University
1990 Champlain Lecturer, Trent
University
1994 Francis
Fraser Lecturer (British Postgraduate Medical Federation, London).
2001 Plenary Lecture Canadian
Health Economics Study Group, Vancouver
2006 Sinclair Lecturer, Queens
University, Kingston
2005 Plenary Lecture, Canadian
Health Economics Study Group, Toronto
University (outside my
Department) Management
1991-94 Pro-Vice-Chancellor, University of
York
1994-97 Deputy Vice-Chancellor
1994-99 Member,
Health Sector Group of the Committee of Vice-Chancellors and Principals
1997-2001 Director of Health Development,
University of York
At
various times Representative of University of York on Court and Council of
Leeds University, 1978-85, member of Council, Nominations Committee, General
Academic Board, Professorial Board, Member or chair of: Staff Committee,
Finance Committee, Secretarial and Clerical Committee, Joint Negotiating
Committee (Joint chair), Court, Council, Appointments to Court and Council,
Vacancies Review Panel, Planning Committee, Administrative Planning Committee,
Policy and Resources Committee, Equipment Subcommittee (minor spenders), VC's
Advisory Group, VC's advisory committees on Academic Plan, Discretionary Salary
Awards; Promotions Committee, Premature Retirement Committee, Leave of Absence
Committee, Research Committee (chair), Awards Sub-Committee (chair), Health
Liaison Group (chair), Board for Graduate Schools (chair), Undergraduate
Admissions Committee (chair), Special Cases Committee (chair), Medical Services
Committee (chair), Library Advisory Committee (chair), Joint Committee with AUT
(chair), Heslington Lectures Committee (chair),
University Committee (chair), King's Manor Resources Group (chair),
Disciplinary Advisory Committee, IT Strategy Committee, Panel for Admin Library
Computing and Other Related Staff (chair), Post-1995 Institutional Planning
Group, Careers Advisory Group (chair), Alcuin Collaboration Group (chair),
Alcuin Project Development Group (chair), Alcuin Project Steering Group
(member), CVCP (in lieu of VC), Search Committee for new VC (1992), chair of
any of the above chaired by VC in his absence, University and University
College of Ripon & York St John Health Collaboration Steering Group
(co-chair).
Principal Canadian Connections
1976 Senior
Research Associate at the Ontario Economic Council and Visiting Professor, Economics
Department, Queens University
1985-6 Visiting Professor, Trent University,
Canada
1986 Woodward Lecturer, University of British Columbia
1989-90 Visiting
Professor, Department of Health Administration, University of Toronto
1989-92 Member,
Methodological Advisory Group on Non-economic Loss, Ontario Workers' Compensation Board
1990 Commissioned to write paper on
Equity in Health for Ontario Premiers Council on Health, Well-Being and Social
Justice
1990 Perey
Lecturer, McMaster
University
1990 Champlain Lecturer, Trent University
1991 (Apr-Sep) Visiting Professor,
Department of Health Administration, University
of Toronto
1990-4
and
1997-02 Member,
Research Advisory Committee, Institute for Work and Health, Toronto
1992-02 Member,
Advisory Committee of the Canadian Institute for Advanced Research Population
Health Program
2000-3 Trustee,
Canadian Health Services Research Foundation, Ottawa
2002-3 Member,
Scientific Advisory Committee, Institute for Work and Health
2003-7 Visiting
professor, Department of Health Policy, Management & Evaluation
, University
of Toronto
2003-6 Chief Scientist,
Institute for Work & Health, Toronto
2003-4 Member, External Research Review Team for
Cancer Care Ontario
2005-7 Adviser, Canada Health Council
2005-6 Member, Ontario Health Technology Advisory Committee
(OHTAC)
2005-7 Member,
CIHR Michael Smith Prize in Health Research Committee
2005- Member, Scientific Committee,
Alberta Bone & Joint Health Institute
2006- Member, International Advisory
Board, Alberta Bone & Joint Institute
2006-7 Senior Scientist,
IWH, Toronto
2006- Advisor to MOHLTC on Citizens
Council
2006- Chair, WSIB Research Advisory
Council
2006-7 Senior Economic Advisor, Cancer
Care Ontario
2007 Chair,
External Review Panel of Centre
for Health Service Policy Research, UBC
2006-10 Chair,
Research Advisory Council, Workplace Safety and Insurance Board (Ontario)
2006-10 Member,
Advisory Board, Centre for Research Expertise in Musculo-Skeletal
Diseases, University of Waterloo
2006-10 Member,
Advisory Board, Centre for Research Expertise in Occupational Disease,
University of Toronto
2006-10 Member,
Advisory Board, Centre for Research Expertise in Improved Disability Outcomes,
University Health Network, Toronto
2006 Member, Ontario
Ministry of Health and Long Term Care Equity
Editorial Board
2007- Member,
Value for Money Committee, Health Council of Canada
2007- Member, Ontario
Ministry of Health and Long Term Care Career Scientist Relevance Review Panel
2007- Member, Ontario Ministry of
Health and Long Term Care Citizens Council Advisory Committee
2007- Member, Ontario Ministry of Health and Long
Term Care Health Research Advisory Council
2008- Chair,
Advisory Committee to CCO Pharmaceutical Economics Unit
2008- Member, Advisory Committee, Toronto Health Economics
and Technology Assessment (THETA) Collaborative
2008- Member, Clinical Standards,
Guidelines and Quality Committee of the Board of Cancer Care Ontario
2009- Member, Interim Scientific
Committee, Occupational Cancer Research Centre, Toronto
2009- Member,
Ontario Ministry of Health and Long Term Care, Health System Strategy Division,
External Advisory Group
2009- Member,
Ontario Ministry of Health and Long Term Care Steering Committee for
Partnerships for Health System Improvement (CIHR project)
2010- Member,
Ontario Health Quality Council Advisory Committee
Current other roles
Co-editor,
Journal of Health Economics
Chair,
Office of Health Economics (London, England)
Adjunct
Scientist, Institute for Work & Health, Toronto
Trustee
and Council member, Royal School of Church Music
Director,
Royal School of Church Music, Canada
Member,
Citizens Council Committee, NICE
Member,
Advisory Committee, NICE International
Member,
MOHLTC Advisory Committee on Citizens Council
Member,
MOHLTC Advisory Committee on R&D
Member,
editorial boards of several other journals
Member,
International Advisory Board, Alberta Bone & Joint Institute
Member,
Advisory Board, Royal
School of Church Music
Member,
Board of Directors, Royal School of Church Music (Canada)
External Assessor
for Chairs etc.
Durham
(economics), Leeds (health economics), London School of Economics (social
policy), London School of Hygiene & Tropical Medicine (health economics)
(twice), Newcastle (health sciences), Oslo (health economics), Toronto (health
economics), Southampton (health policy), UBC (economics) (twice)Northallerton Health Authority (Chief Executive), Office of
Health Economics (deputy director), King's Fund (Chief Executive), National
Institute for Clinical Excellence (Director of Appraisals), North Yorkshire
Health Authority (Director of Primary Care), Director of R&D (NICE).
External Reviews of
Departments
1989 Economics Department, McMaster
University
1993 London Special Health
Authorities (member of Thompson Committee)
1998 Wessex Institute and the Institute of Health Policy,
Southampton University (with Charles Florey) 1
1999 McMaster
University Centre for Health Economics and Policy Analysis (CHEPA)
2007 UBC Centre for Health Services
Policy Research
National Health Service
(England) Appointments
1975-84 Member, DHSS
Research Liaison Groups (several)
1982-90 Member, Northallerton
Health Authority
1990-92 Non-executive member,
Northallerton Health Authority
1991-2001 Member,
Central Research and Development Committee (CRDC) for the National Health
Service
1992-93 Member,
Central R&D Committee Mental Health National Steering Group (Goldberg
Committee)
1992-94 Member, Yorkshire Health Research and
Development Committee
1992-97 Member, CRDC Standing Group on Health
Technology
1993-97 Chair, CRDC Health Technology
Assessment (HTA) Methodology Panel
1992-93 Member,
Review Advisory Committee on the London Special Health Authorities. (The
"Thompson Report, Special Health Authorities: Research Review, London,
HMSO, 1993, chaired by Sir Michael Thompson)
1993-94 Chair,
NHS Research Task Force on R&D to Review the Funding and Support of
Research and Development in the NHS, (The "Culyer Report): Supporting Research and Development in the
NHS: A Report to the Minister of Health, London, HMSO, 1994
1994-99 Deputy
Chair and non-executive member, North Yorkshire Health
Authority
(reappointed to new Authority in 1996), (chair and member of several
subcommittees of the Board)
1995-2001 Member, Northern & Yorkshire Regional
Research Advisory Group
1995-2001 Member, Northern and Yorkshire Regional
Universities Group for R&D
1995-99 Special
Adviser, High Security Psychiatric Services Commissioning Board (HSPSCB)
1995-1999 Member, R&D Committee of the HSPSCB
1995-99 Member, R&D Commissioning Sub
Group of the HSPSCB
1996 Member,
Central R&D Committee Sub-Group on the Strategic Framework
1996-97 Member,
National Working Group on R&D in Primary Care (Mant
Committee)
1997-98 Chair,
Department of Health Expert Workshop on DH Guidelines for Pharmaco-economic
studies
1997-98 Adviser,
Department of Health Comprehensive Spending Review Group on "Non
front-line services"
1997-99 Special Adviser
to NHS Director of R&D
1997-98 Chair,
Central R&D Committee Sub-Group on Budget 1 Allocations to Trusts
1998-2002 Member,
Healthcare Sector Group, Department of Trade and Industry and Department of
Health Overseas Trade Services
1998-2000 Member, NHS R&D Exceptional Cases
Advisory Group
1998-2000 Member, NHS R&D Strategic Review Sub
Group
1998-2000 Member, NHS R&D Evaluation Strategy
Steering Group
1999-2003 Vice
Chair (and non-executive director), National Institute for Clinical Excellence
2007-10 Chair, NICE
Research & Development Committee
2007- Member, NICE
Citizens Council Committee
2008- Member, NICE
International Advisory Committee
2008 Member,
Department of Health Value Focus Group on the cost and benefit perspective of
NICE
Other
Government roles
1983-87 Member, Comac-HSR
Committee of the European Commission
1995-97 Member, British Council Health
Advisory Committee
1997-98 Member,
Department of Trade and Industry Advisory Committee on Exports of Health-related
Products
2005-07 Member, Economics Advisory Panel,
Home Office
Recent
publications (2007-10)
2007
Culyer A J. Need - an
instrumental view in Richard Ashcroft, Angus Dawson, Heather Draper and John
McMillan (Eds.) Principles of Health Care
Ethics, 2nd Edition, Chichester: Wiley, 2007, 231-238.
Culyer
A J. When and how cancer chemotherapy should be privately funded," Oncology Exchange, 2007, 6: 47.
Culyer A J, McCabe C, Briggs AH,
Claxton K, Buxton M, Akehurst RL, Sculpher M and Brazier J. Searching for a
threshold, not setting one: the role of the National Institute of Health and
Clinical Excellence, Journal of Health
Service Research and Policy, 2007, 12: 56-59.
Robson
LS, Clarke J, Cullen K, Bielecky A, Severin C, Bigelow P, Irvin E, Culyer AJ, Mahood Q. The
Effectiveness of Occupational Health and Safety Management System
Interventions: A Systematic Review, Safety
Science, 2007, 45: 329-353.
Culyer A J Merit goods and the welfare economics of coercion in Wilfried Ver Eecke (Ed.) Anthology regarding Merit Goods. The Unfinished
Ethical Revolution in
Economic Theory. West Lafayette: Purdue University
Press, 2007, 174-200 (reprinted from Public
Finance, 1971, 26: 546-572.
Claxton K and Culyer A J,
Rights, responsibilities and NICE: A Rejoinder to Harris Journal of Medical Ethics, 2007, 33: 462-464.
Culyer A J, NICE misconceptions The Lancet, September 11 2007, on-line at http://www.thelancet.com/journals/lancet/article/PIIS014067360761321X/comments
Culyer A J, Equity of what in health care? Why
the traditional answers don't help policy - and what to do in the future HealthcarePapers, 2007,
8(Sp): 12-26.
Culyer A J, McCabe C, Briggs
A, Claxton K, Buxton M, Akehurst
R, Sculpher M, Brazier J, Searching
for a threshold - Not so
, Journal of Health Services
Research and Policy, 2007, 12:
190-191. (letter: reply to G Mooney, J Coast, S
Jan, D McIntyre, M Ryan and V Wiseman).
Culyer A J, Resource allocation in health care:
Alan Williams decision maker, the
authority and Pareto, in A Mason & A Towse (eds.) The
Ideas and Influence of Alan Williams:
Be Reasonable Do it My Way! Oxford,
Radcliffe Publishing, 2007, 57-74.
2008
E Tompa, A J Culyer, R Dolinschi (Eds.) Economic Evaluation of Interventions for
Occupational Health and safety: Developing Good Practice, Oxford: Oxford University Press, 2008, pp.
xvi + 295.
Chalkidou K, Culyer A J, Naidoo B, Littlejohns P Cost-effective
public health guidance: asking questions from the decision-maker's
viewpoint, Health Economics,
2008, 17: 441-448.
Claxton K, Briggs A, Buxton M, Culyer A J, McCabe C, Walker S,
Sculpher M J Value based pricing for
NHS drugs: an opportunity not to be missed? British Medical Journal,
2008, 336: 251-254.
Brouwer W B F, Culyer A J, Job N,
van Exel A, Rutten F
F H. Welfarism vs. extra-welfarism, Journal of Health Economics, 2008, 27: 325338.
J Hurley, D Pasic, J Lavis, A
J Culyer C Mustard and W Gnam, Parallel payers and preferred access: how
Canadas Workers Compensation Boards expedite care for injured and ill
workers, HealthcarePapers,
2008, 8: 6-14.
J Hurley, A J Culyer, W Gnam, J Lavis, C Mustard and D
Pasic, Response to commentaries, HealthcarePapers, 2008, 8: 52-54.
K Chalkidou, T Walley, A J Culyer, P Littlejohns, and A Hoy. Evidence-informed
evidence-making, Journal of Health
Services Research & Policy, 2008, 13: 167-173.
K Claxton and A J Culyer Not a NICE fallacy: A reply to Dr Quigley, Journal of Medical Ethics 2008, 34:
598-601.
A J Culyer, B Amick and A LaPorte. What is a little more health and safety worth?
in E Tompa, A J Culyer, R Dolinschi (Eds.) Economic Evaluation of Interventions for
Occupational Health and safety: Developing Good Practice, Oxford: Oxford University Press, 2008, 15-35.
A J Culyer and M Sculpher. Lessons from health technology
assessment in E Tompa, A J Culyer,
R Dolinschi (Eds.) Economic Evaluation of
Interventions for Occupational Health and safety: Developing Good Practice,
Oxford: Oxford
University Press, 2008, 51-69.
A J Culyer
and E Tompa.
Equity, in E Tompa, A J Culyer, R Dolinschi (Eds.) Economic
Evaluation of Interventions for Occupational Health and safety: Developing Good
Practice, Oxford:
Oxford University Press, 2008, 215-231.
E Tompa, A J Culyer and R Dolinschi
Suggestions for a reference case, in E Tompa, A J Culyer, R Dolinschi (Eds.) Economic
Evaluation of Interventions for Occupational Health and safety: Developing Good
Practice, Oxford:
Oxford University Press, 2008, 235-244.
C McCabe, K Claxton and A J Culyer The NICE
cost effectiveness threshold what it is and what that means, PharmacoEconomics,
2008,
26: 733-744.
K Chalkidou, A J Culyer, P Littlejohns, P Doyle, A Hoy. Imbalances in funding for clinical and public health
research in the UK:
can NICE research recommendations make a difference? Evidence and Policy, 2008, 4: 355-369.
J Hurley, D
Pasic, J Lavis, C Mustard, A J Culyer,
W Gnam. Parallel
lines do intersect: interactions between the workers compensation and
provincial
publicly financed health care systems in Canada. HealthCare Policy, 2008, 3: 100-112.
2009
Chalkidou K, A J
Culyer, B Naidoo, P Littlejohns "The challenges of developing
cost-effective public health guidance: a NICE perspective", in S Dawson
and Z S Morris (eds.) Future Public
Health: Burdens, Challenges and Opportunities, Basingstoke:
Palgrave Macmillan, 2009, 276-291.
A J Culyer, Deliberative
Processes in Decisions about Health Care Technologies: Combining Different
Types of Evidence, Values, Algorithms and People, London: Office of Health
Economics, 2009, pp. 1-20.
A J Culyer How
Nice is NICE? A Conversation with Anthony Culyer, Health Care Cost
Monitor, Hastings Centre Blog, 2009.
M. J. Dobrow, R. Chafe, H. E. D. Burchett, A J Culyer, L. Lemieux-Charles Designing Deliberative Methods for Combining Heterogeneous Evidence: A
Systematic Review and Qualitative Scan. A Report to the Canadian Health
Services Research Foundation, Ottawa:
Canadian Health Services Research Foundation, 2009, pp. 24 + 30, ().
2010
Cookson
R, A J Culyer. Measuring overall population health - the use
and abuse of QALYs, in Killoran A, Kelly M (eds). Evidence
Based Public Health: Effectiveness and Efficiency, Oxford: Oxford
University Press, 2010, 148-168.
A J Culyer, The Dictionary of Health Economics,
Cheltenham: Edward Elgar, 2010.
A J Culyer "Perspective and desire in comparative effectiveness research - the relative unimportance of mere preferences, the central importance of context", Pharmacoeconomics, 28: 1-9.
2011
K Claxton, M
Paulden, H Gravelle, W Brouwer, A J
Culyer. Discounting and decision making in the
economic evaluation of health-care technologies, Health Economics, 2011, 20: 2-15.
R Chase, A J Culyer, M Dobrow, P Coyte, C Sawka, S OReilly, K Laing, M
Trudeau, S Smith, J Hoch, S Morgan, S Peacock, R Abbott, T Sullivan. Access to
Cancer Drugs in Canada: Looking Beyond Coverage Decisions, Healthcare Policy, 2011, 6: 27-35.
A J Culyer. UK report: NHS
reforms, Health Care Cost Monitor,
2011, 1-2. The Hastings Centre, on-line at http://healthcarecostmonitor.thehastingscenter.org/anthonyculyer/u-k-report-nhs-reforms.
P Tso, A J
Culyer, M Brouwers, M J Dobrow. Developing a
decision aid to guide public sector health policy decisions: A study protocol,
Implementation Science, 2011, 6:46.
Current
grants
Strengthening the health system
through improved priority setting. Canadian Institutes of Health Research
(Sustainable Financing, Funding and Resource Allocation), Co-investigators: Dr.
Andreas Laupacis
(PI), Dr. Doug Martin (Co-PI_, Dr.
W. Evans, Dr. W. Levinson, Dr. T. Sullivan, Dr. S. Pearson, Dr. A. Hudson.
$159,805 per year for 5 years, 04/2005 to 09/2010.
Dynamics of Parallel Systems of Finance:
Interactions Between Canada's Worker Compensation
Systems and Public Health Care Systems; Canadian Institutes of Health Research.
Co-investigators: Dr Jerry Hurley
(PI), Dr William Gnam, Dr John Lavis, Dr Cameron
Mustard, Dr Emile Tompa.
$75,000 for 1 year, Reference #: PPG-74820.
Several grant applications to CIHR with M
Dobrow (Cancer Care Ontario)
and others are currently being considered.
Recent
grant
Conceptualising and Combining
Evidence for Health System Guidance, Canadian Institutes of Health Research,
Co-investigator Dr Jonathan Lomas,
2005.
Teaching
Experience
Graduate
At various times have given lectures and
seminars in Advanced Economic Theory (micro and macro), the Economics of Human
Resources, the Economics of Social Policy, Health Economics, Social Policy
Analysis, and given graduate classes on Social Policy to students of Social
Administration. Supervised MSc, MPhil and DPhil thesis students.
PhD external examiner at various Universities in the UK and
overseas.
Undergraduate
At various times have given first year
introductory lectures in Economics; second year lectures in Price Theory,
Welfare Economics, Macroeconomics, and Investment Appraisal; third year
lectures and seminars in Economics of the Social Services, Economics of Human
Resources, Health Economics, Applied Economics, and Advanced Economic Theory. External examining.
Listed
in
At various times:
Who's Who in Economics: A Biographical
Dictionary of Major Economists 1700-1981 (ed. Blaug
and Sturges), Wheatsheaf,
1983 (and subsequent editions)
Who's Who
Who's Who in Education
Whos Who in America
Whos Who in the World
The Academic Who's Who
The Universities' Who's Who
The International Authors' and Writers' Who's
Who
People of Today
Recreation
and other
Church music: Emeritus Organist and Choir
Director in an Anglican rural parish church in England, Chair of the York
District of the Royal School of Church Music 1983-95, Chair of North East Area
Committee of the Royal School of Church Music 1995-2003, member RSCM Advisory
Board 2002-4, Member of Council and Trustee RSCM, 2003-. Board
Director of Royal School of Church Music (Canada) 2008-. Member of the York Diocesan Liturgy and
Music Advisory Group 1995-99. Various roles in local Church of England (at various
times Parochial Church Council member, Lay Chair of Parochial Church Council,
Sometime Deanery Financial Adviser, Sometime Member York Diocesan Church Urban
Fund, etc.). Amateur composer. Music
generally. Gardening when time, weather and low back problems permit.
DIY when time and LBP permit and urgency insists.
PUBLICATIONS
A.
Articles
1.
A J Culyer. "Methodological error in
regional planning: the South West Strategy", Social and Economic Administration, 1968, 2: 23-30.
2.
A J Culyer. "Holidays on the move", New Society, 11 April, 1968.
3.
A J Culyer, D C Corner "University
teachers and the PIB", Social and
Economic Administration, 1969, 3:
127-139.
4.
F
M M Lewes, A J
Culyer, G A Brady. "The holiday industry" in British Association,
Exeter and its Region, Exeter: University
of Exeter. 1969, 244-258.
5.
A J Culyer. "Pricing policies" in G. Teeling-Smith (ed.), Economics
and Innovation in the Pharmaceutical Industry, London: Office of Health Economics, 1969,
35-50.
6.
A J Culyer. "The economics of health
systems" in The Price of Health,
Melbourne: Office of Health Care Finance, 1969, 36-62 (reprinted as ch.7 in J.
R. G. Butler and D. P. Doessel (eds.), Health Economics: Australian Readings,
Sydney: Australian Professional Publications, 1989, 145-66).
7.
M
H Cooper, A J Culyer. "An
economic assessment of some aspects of the organisation
of the NHS" in BMA, Health Services
Financing, London:
British Medical Association, 1970, 187-250.
8.
A J Culyer. "A utility-maximising
view of universities", Scottish Journal
of Political Economy, 1970, 17:
349-68.
9.
A J Culyer, A K Maynard. "The cost of
dangerous drugs legislation in England
and Wales",
Medical Care, 1970, 8: 501-509.
10.
M
H Cooper, A J Culyer. "An
economic survey of the nature and intent of the British National Health
Service", Social Science and
Medicine, 1971, 5: 1-13.
11.
A J Culyer. "Ethics and economics in blood
supply", Lancet (i) March 1971.
12.
A J Culyer. "Social scientists and blood
supply", Lancet (i) June 1971.
13.
A J Culyer. "The nature of the commodity
'health care' and its efficient allocation", Oxford Economic Papers, 1971,
23: 189-211 (reprinted as Ch. 2 in
A. J. Culyer and M. H. Cooper (eds.), Health
Economics, London: Penguin, 1973, also in A J Culyer (Ed.) Health Economics: Critical Perspectives on
the World Economy, London: Routledge, 2006,
148-157).
14.
A J Culyer. "Medical care and the
economics of giving", Economica, 1971, 38:
295-303 (reprinted as Ch. 18 in M. Ricketts (ed.), Neoclassical Microeconomics, Vol. 2, Aldershot:
Edward Elgar, 1989, pp. 310-18).
15.
A J Culyer. "A taxonomy of demand
curves", Bulletin of Economic
Research, 1971, 23: 3-23.
16.
A J Culyer. "Calculus of health", New Society, 23 September, 1971.
17.
A J Culyer, A Williams, R J Lavers. "Social
indicators: health", Social Trends,
1971, 2: 31-42 (reprinted as Health indicators in
Andrew Shonfield and Stella Shaw (eds.) Social Indicators and Social Policy, London: Heinemann, 1972).
18. A J Culyer.
"Merit goods and the welfare economics of coercion", Public Finance, 1971, 26:
546-72. (Reprinted in Wilfried
Ver Eecke
(2006) Merit Goods: The Birth of a New
Concept. The Unfinished Ethical Evolution in Economic Theory. Ashland Ohio: Purdue University
Press, 174-200).
19.
A J Culyer. "Appraising government spending
on health services: The problems of 'need' and 'output'", Public Finance, 1972, 27: 205-11.
20.
A J Culyer. "On the relative efficiency of
the National Health Service", Kyklos, 1972, 25: 266-287.
21.
A J Culyer."The market versus the state
in medical care: a minority report on an empty academic box", in G.
McLachlan (ed.), Problems and Progress in
Medical Care, 7, London:
Oxford University Press, 1972, 1-32.
22.
M
H Cooper, A J Culyer. "Equality
in the NHS: intentions, performance and problems in evaluation", in M. M.
Hauser (ed.), The Economics of Medical
Care, London:
Allen and Unwin, 1972, 47-57.
23.
A J Culyer, A Williams, R J Lavers. "Social
indicators: health" in A. Shonfield and S. Shaw
(eds.) Social Indicators and Social
Policy, London, Heinemann, 1972, (reprint of 1971 article in Social Trends).
24.
A J Culyer. "Comment on Problems of
Efficiency", in M. M. Hauser, Hauser (ed.), The Economics of Medical Care, London: Allen and Unwin,
1972, 42-46
25.
A J Culyer, P Jacobs. "The War and public
expenditure on mental health - the postponement effect", Social Science and Medicine, 1972, 6: 35-56.
26.
A J Culyer. "Indicators of health: an
economist's viewpoint ", in Evaluation
in the Health Services, London:
Office of Health Economics, 1972, 23-28.
27.
A J Culyer. "Lefficienza relativo del
Servizio Sanitario Nazionale Brittanico", Citta e Societa, 1972, March/April, 35-53.
28.
A J Culyer. "Social policy and government
spending", Local Government Finance,
1972, 76: 353-357.
29.
A J Culyer. "Economic analysis - its
practice and pitfalls", Local
Government Finance, 1972, 76:
385-389.
30.
A J Culyer. "Pareto, Peacock and Rowley,
and the public regulation of natural monopoly", Journal of Public Economics, 1973, 2: 89-95.
31.
A J Culyer. "Should social policy concern
itself with drug 'abuse'?", Public
Finance Quarterly, 1973, 1:
449-456.
32.
A J Culyer. "Hospital waiting lists",
New Society, 16 August, 1973.
33.
A J Culyer. "Is medical care
different?" in A. J. Culyer and M. H. Cooper (eds.) Health Economics, London:
Penguin, 1973, 49-74 [reprint with changes of 1971 article in Oxford Economic
Papers].
34.
A J Culyer. "Hospital waits", New Society, 6 December, 1973.
35.
A J Culyer. "Quids
without quos - a praxeological approach", in A.
A. Alchian et
al. The Economics of Charity, London: IEA, 1973, 35-61.
36.
M
H Cooper, A J Culyer. "The
economics of giving and selling blood", in A. A. Alchian
et al. The Economics of Charity, London, IEA, 1973,
111-143.
37.
J
G Cullis, A J
Culyer. "Private patients in NHS hospitals: subsidies and waiting
lists", in M. Perlman (ed.), The
Economics of Health and Medical Care, International Economics Association.,
London:
Macmillan, 1974, 108-116.
38.
A J Culyer. "Economics, social policy and
disability", in Dennis Lees and Stella Shaw (eds.), Impairment, Disability and Handicap, London: Heinemann for the SSRC, 1974, 17-29.
39.
A J Culyer. "Dialogue on blood 1", New Society, 24 March, 1974.
40.
A J Culyer. "Hospitals",
New Society, 20 June, 1974.
41.
A J Culyer. "Introduction" to University Economics, (3rd Ed.) by A. A.
Alchian and W. R. Allen, Prentice-Hall International,
1974.
42.
R
L Akehurst, A
J Culyer. "On the economic surplus and the value of life", Bulletin of Economic Research, 1974, 26: 63-78
43.
A J Culyer. "The economics of health"
in R. M. Grant and G. K. Shaw (eds.),
Current Issues in Economic Policy, London:
Philip Allan, 1975, 151-173.
44.
A J Culyer. "Value for money in
health", New Society, March
1975.
45.
A J Culyer, J G Cullis.
"Hospital waiting lists and the supply and demand of inpatient care",
Social and Economic Administration,
1975, 9: 13-25.
46.
A J Culyer, J Wiseman, J Posnett.
"Charity and public policy in the U.K.: the law and the
economics", Social and Economic
Administration, 1976, 10: 32-50.
47.
J
G Cullis, A J
Culyer. "Some economics of hospital waiting lists in the NHS", Journal of Social Policy, 1976, 5: 239-264.
48.
A J Culyer. "Discussion of 'Health Costs
and Expenditures in the U.K.'
by M. H. Cooper", in Tei-wei Hu
(Ed.) International Health Costs and
Expenditures, Washington
D.C.: U.S. Department of Health
Education and Welfare, 1976, 109-113.
49.
A J Culyer. "Alternatives to price
rationing: some unsolved riddles for British health economists", in R. D.
Fraser (ed.), Health Economics Symposium,
Proceedings of the First Canadian Conference, Kingston
(Ontario):
Industrial Relations Centre, Queen's University, 1976, 66-74.
50.
A J Culyer, J Wiseman. "Public economics
and the concept of human resources", in Victor Halberstadt
and A. J. Culyer (eds.) Human Resources
and Public Finance, (eds.), Paris: Cujas, 1977, 13-29.
51.
A J Culyer. "Blood and altruism: an
economic review", in D. B. Johnson (ed.), Blood Policy - Issues and Alternatives, Washington
D.C: American Enterprise Institute, 1977, 39-58.
52.
A J Culyer. "The quality of life and the
limits of cost-benefit analysis", in L. Wingo
and A. Evans (eds.), Public Economics and
the Quality of Life, Baltimore:
Johns Hopkins, 1977, 141-153.
53.
A J Culyer. "Drugs and Pareto - a
methodological abuse", Public Finance
Quarterly, 1977, 5: 393-396.
54.
A J Culyer. "Need, values and health
status measurement", in A. J. Culyer and K. G. Wright (eds.), Economic Aspects of Health Services,
London: Martin Robertson, 1978, 9-31.
55.
M
F Drummond, A J Culyer.
"Financing medical education - interrelationships between medical school
and teaching hospital expenditure", in A. J. Culyer and K. G. Wright
(eds.), Economic Aspects of Health
Services, London: Martin Robertson, 1978, 123-140.
56.
A J Culyer, J. Wiseman, M. F. Drummond, P. A.
West. "What accounts for the higher costs of teaching hospitals?" Social and Economic Administration,
1978, 12: 20-30.
57.
A J Culyer. "Economics and the health
services: missionary role of economists", Surgical News, No. 5, Summer 1978, 2-4.
58.
A J Culyer. "Editorial", Epidemiology and Community Health, 1979,
33: .
59.
A J Culyer. Comment on Theories and
Measurement in Disability by R. G. A. Williams, Epidemiology and Community Health, 1979, 33: .
60.
A J Culyer. "Into the valley: review
article of 'Charge' by A. Seldon", Social Policy
and Administration, 1979, 13: 65-68.
61.
A J Culyer. "What do health services do
for people?" Search, 1979, 10: 262-268.
62.
A J Culyer, J Wiseman. "Frameworks for
evaluating economic effects of budget and financial transfers in the EEC",
in Study Group on the Economic Effects of
Budget and Financial Transfers in the Community, Part II, Brussels,
Commission of the European Communities, 1979.
63.
A J Culyer. "Cost-sharing: financial
aspects and policies", in B. Abel-Smith (ed.), Sharing Health Care Costs, Washington D.C.:
National Center for Health Services Research;
U.S. Department of Health, Education and Welfare, 1980, 18-19.
64.
A J Culyer. "Economics and the health
services", in R. M. Grant and G. K. Shaw (eds.), Current Issues in Economic Policy, 2nd ed., London: Philip Allan,
1980, 164-186.
65.
A J Culyer, A K Maynard. Treating ulcers with Cimetidine can be more cost-effective than surgery", Medeconomics,
1980 1: 12-14.
66.
A J Culyer. "Externality models and
health: a Rückblick over the last twenty years",
in P. M. Tatchell (ed.), Economics and Health: Proceedings of the First Australian Conference of
Health Economists, Canberra: Australian National
University Press, 1980, 139-157. (reprinted with changes in The Economic Record, 1980, 56:
222-30).
67.
A J Culyer. Discussion of Universality and
Selectivity in the Targeting of Government Health/Welfare Programs by D. Dixon in P. M. Tatchell (ed.), Economics and Health: Proceedings of the
First Australian Conference of Health Economists, Canberra, Australian National
University Press, 1980,
11-17.
68.
A J Culyer, Heather Simpson. "Externality
models and health: a Rückblick over the last twenty
years", The Economic Record,
September 1980, 56: 222-30. (Reprint with changes in P. M. Tatchell
ed., Economics and Health: Proceedings of
the First Australian Conference of Health Economists, Canberra: Australian
National University Press, 1980, 139-157).
69.
A J Culyer, M. Pfaff, H. Hauser. "Report on financial aspects and policies"
in A. Brandt, B. Horisberger and W. P. von Wartburg
(eds.), Cost-Sharing in Health Care, Heidelberg: Springer,
1980.
70.
A J Culyer, A K Maynard.
"Cost-effectiveness of duodenal ulcer treatment", Social Science and Medicine, 15C, 3-11,
1981. (Reprinted in shortened form in Bernard S. Bloom (ed.), Cost-Benefit and Cost-Effectiveness Analysis
in Policymaking. Cimetidine as a Model, New York: Biomedical
Information Corporation, 1982, 128-31).
71.
A J Culyer. "The IEA's unorthodoxy",
in R. Harris and A. Seldon (eds.), The Emerging Consensus
...? London:
Institute of Economic Affairs, 1981, 99-119.
72.
A J Culyer. "Acht Trugschlüsse über das britische
Gesundheitswesen", Medita, 1981,
6: 22-27.
73.
A J Culyer. "European workshop on health
indicators: a draft report", Revista Internacional de Sociologi,
1981, 39: 151-171.
74.
A J Culyer. "Economics, social policy and
social administration: the interplay between topics and disciplines", Journal of Social Policy, 1981, 10: 311-29.
75.
A J Culyer. "Health, economics and health economists"
in J. Van de Gaag and M. PerIman
(eds.), Health Economics and Health
Economists, Amsterdam:
North-Holland, 1981.
76.
A J Culyer. "Economics, health and health
services" in R. Clara et al, Health
and Economy, Part 1, Antwerp: Antwerp University Press, 1981, 19-33.
77.
A J Culyer, A K Maynard.
"Cost-effectiveness of duodenal ulcer treatment", in Bernard S. Bloom
(ed.) Cost-Benefit and Cost-Effectiveness
Analysis in Policymaking: Cimetidine as a Model, New York: Biomedical
Information Corporation, 1, 128-13. (Reprint of 1981 Social Science and Medicine article).
78.
A J Culyer, A K Maynard, A
H Williams. "Alternative systems of health care provision: an essay on
motes and beams" in Mancur Olson (ed.), A New Approach to the Economics of Health
Care, Washington:
American Enterprise Institute, 1982, 131-150.
79.
A J Culyer, J Wiseman, M F Drummond, P A West.
"Revenue allocation by regression: a rejoinder", Journal of the Royal Statistical Society, Series A, 1982, 145: Part 1, 127-33.
80.
A J Culyer. "Health services in the mixed
economy" in Lord Roll of Ipsden (ed.), The Mixed Economy, London, Macmillan,
1982, 128-144. (reprinted in Magyar as "Egeszsegugyi szolgaltatasok a vegyes gazdasagban", Esely, 9113,
1991, 37-48).
81.
A J Culyer. "Egeszsegugyi
szolgaltatasok a vegyes gazdasagban", Esely, 9113, 1991, 37-48).
82.
T
Sandler, A J Culyer. "Joint
products and multi-jurisdictional spillovers", Quarterly Journal of Economics, 1982, 97: 707-716.
83.
A J Culyer. "Assessing
cost-effectiveness", in H. D. Banta (ed.), Resources for Health: Technology Assessment for Policy Making, Westport: Praeger, 1982, 107-120.
84.
A J Culyer. "The NHS and the market:
images and realities", in G. McLachlan and A. Maynard (eds.), The Public/Private Mix for Health: the
Relevance and Effects of Change, London, Nuffield Provincial Hospitals
Trust, 1982, 25-55.
85.
A J Culyer. "Health care and the market: a
British lament, Journal
of Health Economics, 1982, 1: 299-303.
86.
T
Sandler, A J Culyer. Joint products
and multi-jurisdictional spillovers: some public goods geometry", Kyklos, 1982, 35: 702-9.
87.
A J Culyer. "A Hatekonysag
Keresese a Kozuleti Szektorban: Kozgadzak contra dr. Pangloss" (trs. from English by Otto Gado), Penziigyi Szemle, 27,
1983, 378-384.
88.
A J Culyer. "Introduction" to Health
Indicators, ed. A. J. Culyer, London,
Martin Robertson, 1983, 1-22.
89.
A J Culyer. "Conclusions and
recommendations" in A. J. Culyer (Ed.) Health
Indicators, London:
Martin Robertson, 1983, 186-193.
90.
A J Culyer. "Effectiveness and efficiency
of health services", Effective
Health Care, 1983, 1: 7-9.
91.
A J Culyer, J. MacFie,
A. Wagstaff. "Cost-effectiveness of foam elastomer
and gauze dressings in the management of open perineal
wounds", Social Science and Medicine,
1983, 17: 1047-53.
92.
A J Culyer. "Public or private health
services: a skeptic's view", Journal
of Policy Analysis and Management, 1983, 2: 386-402.
93.
A J Culyer. "The marginal approach to
saving lives", Economic Review,
1, 1983, 21-23.
94.
A J Culyer. "Economics without economic
man?" Social Policy and
Administration, 1983, 17: 188-203.
95.
A J Culyer, B Horisberger.
"Medical and economic evaluation: a postscript" in A. J. Culyer and
B. Horisberger (eds.), Economic and Medical Evaluation of Health Care Technologies, Heidelberg: Springer,
1983, 347-358. (Also published separately by the same publishers in German).
96.
A J Culyer. "La contribución del Análisis
Económico a la Pólitica Social ", in J-J. Artells (ed.), Primeres Jornades dEconomia dels Serveis
Socials, Barcelona, Impres Layetana, 1983, 17-34.
97.
A J Culyer. "Marco para la evaluación
multidisciplinaria de los servicios sociales", in J-J. Artells (ed.), Primeres Jornades dEconomia dels
Serveis Socials, Barcelona, Impres Layetana, 1983, 35-39.
98.
A J Culyer, A
Wagstaff, J MacFie. "Foam elastomer
and gauze dressings in the management of open perineal
wounds: a cost-effectiveness study", British
Journal of Clinical Practice, 1984, 38:
263-8.
99.
A J Culyer, J Posnett.
"Profit regulation in the drug industry: a bitter pill?",
Economic Review, 1984, 2:
19-21.
100.
A J Culyer. "The quest for efficiency in
the public sector: Economists versus Dr. Pangloss (or
why conservative economists are not nearly conservative enough)", in H. Hanusch (ed.), Public
Finance and the Quest for Efficiency, Proceedings of the 38th Congress of
the UPF, Copenhagen, Detroit, Wayne State University Press, 1984, 39-48.
101.
A J Culyer, J Posnett.
"Would you choose the Welfare State?" Economic Affairs, 1985, 5: 40-42.
102.
A J Culyer. "What's wrong with economics
textbooks?",
Economics, 1985, 21: 15-17.
103.
A J Culyer. "A health economist on medical
sociology: reflections by an unreconstructed reductionist, Social Science and Medicine, 1985, 20: 1013-21.
104.
A J Culyer. "On being right or wrong about
the welfare state", in P. Bean, J. Ferris and D. Whynes
(eds.), In Defence
of Welfare, London:
Tavistock, 1985, 122-41.
105.
A J Culyer. "Discussion" in N. Wells
(ed.), Pharmaceuticals among the Sunrise Industries, London: Croom Helm,
1985, 218-224.
106.
A J Culyer, S Birch. "Caring for the
elderly: a European perspective on today and tomorrow", Journal of Health Politics, Policy and Law,
1985, 10: 469-87.
107.
A J Culyer. "What dangers from medical
monopoly?" Economic Affairs,
1986, 6: 56-7.
108.
A J Culyer. "The scope and limits of
health economics (with reference to economic appraisals of health
services)" in Oekonomie des Gesundheitswesen,
Jahrestagung des Vereins für Socialpolitik, Gesellschaft für Wirtschafts- und Sozialwissenschaften,
Neue Folge Band 159, 1987,
Berlin: Duncker & Humblot,
31-53.
109.
A J Culyer. "The future of health
economics in the U.K.
", in Health Economics: Prospects
for the Future, ed. G. Teeling Smith, London: Croom Helm, 1987, 15-32.
110.
A J Culyer. "Assessing the costs and
benefits of pharmaceutical research", in G. Teeling
Smith (ed.), Costs and Benefits of
Pharmaceutical Research, London:
Office of Health Economics, 1987, 25-27.
111.
A J Culyer, C Blades, A
Walker.
"Health service efficiency, appraising the appraisers - a critical review
of economic appraisal in practice", Social
Science and Medicine, 1987, 25,
461-72.
112.
A J Culyer. "Technology assessment in
Europe: its present and future roles", in E E H.
Rutten and S. J. Reiser
(eds.), The Economics of Medical
Technology, Berlin:
Springer, 1987, 54-79.
113.
A J Culyer. "Health economics: the topic
and the discipline", in J. M. Horne (ed.), Proceedings of the Third Canadian Conference on Health Economics, 1986,
Winnipeg: Department of Social and Preventive
Medicine, University of Manitoba,
1987, 1-18.
114.
A J Culyer. "Discussion of R. G. Evans et
al, Toward efficient aging: rhetoric and
evidence", in J. M. Horne (ed.), Proceedings
of the Third Canadian Conference on Health Economics, 1986, Winnipeg: Department of Social and Preventive Medicine,
University of Manitoba,
1987, 170-1.
115.
A J Culyer. "Inequality of health services
is, in general, desirable", in D. Green (ed.), Acceptable Inequalities? Institute of Economic Affairs, London: 1988, 31-47.
116.
A J Culyer. "The radical reforms the NHS needs
- and doesn't", Minutes of Evidence
Taken before the Social Services Committee, London: HMSO, 1988, 238-242.
117.
A J Culyer. Comments on Public
Hospital Performance Assessment by
Arthur Andersen and Co., in Response From the Hospital Boards' Association of New Zealand to "Unshackling the Hospitals
the Report of the Hospital and Related Services Taskforce, Hospital Boards'
Association, New Zealand,
1988.
118.
A J Culyer. "Medical care and the
economics of giving", in M. Ricketts (ed.) Neoclassical Microeconomics, vol. 2, Aldershot: Edward
Elgar, 1988, 310-318 (reprint of 1971 article in Economica).
119.
A J Culyer. "The normative economics of
health care finance and provision", Oxford Review of Economic Policy, 5, 1, 1989,
34-58. (reprinted with changes in A. McGuire, P. Fenn and K. Mayhew (eds.) Providing Health Care: The Economics of
Alternative Systems of Finance and Delivery, Oxford: Oxford University Press, 1991, 65-98,
also in A J Culyer (Ed.) Health
Economics: Critical Perspectives on the World Economy, London: Routledge,
2006, 148-157)
120.
A J Culyer. "Commodities, characteristics
of commodities, characteristics of people, utilities and the quality of
life", in S. Baldwin, C. Godfrey and C. Propper (eds.), The
Quality of Life: Perspectives and Policies. London: Routledge,
1989, 9-27. (Reprinted 1994)
121.
A J Culyer. "The economics of health
systems", in R. G. Butler and D. P. Doessel
(eds.) Health Economics: Australian
Readings, Sydney: Australian Professional Publications, 1989, 145-166
(reprint of 1969 article in The Price of Health).
122.
A J Culyer. "Implications of the
Ministerial Review of the NHS", in Opportunities
for the Independent Sector: Articles from the NHS Review, Annual Conference
Review, Independent Hospitals Association, 1989, 6-9.
123.
A J Culyer. "A glossary of the more common
terms encountered in health economics", in M. S. Hersh-Cochran
and K. P. Cochran (eds.), Compendium of
English Language Course Syllabi and Textbooks in Health Economics,
Copenhagen: WHO, 1989, 215-234.
124.
A J Culyer. "Cost containment in Europe", Health
Care Financing Review, Annual Supplement, 1989, 21-32. (reprinted
in Health Care Systems in Transition,
Paris: OECD, 1990.)
125.
A J Culyer. "Competition and markets in
health care: what we know and what we don't, Part I", Cardiology Management, 1990, 3: 15-18.
126.
A J Culyer. "Competition and markets in
health care: what we know and what we don't, Part II ", Cardiology
Management, 1990, 3: 36-38.
127.
A J Culyer. "Cost containment in Europe", in Health
Care Systems in Transition, Paris: OECD, 1990, 000-000. (Reprint of 1989
article in Health Care Financing Review ).
128.
A J Culyer, B Luce, A
Elixhauser. "Socioeconomic evaluations: an
executive summary ", in Culyer (ed.), Standards
for Socioeconomic Evaluation of Health Care Products and Services, Berlin:
Springer, 1990, 1-12.
129.
A J Culyer, J W Posnett.
"Hospital behaviour and competition", in A. J. Culyer, A. K. Maynard
and J. W. Posnett (eds.), Competition in Health Care: Reforming the NHS, London: Macmillan,
1990, 12-47.
130.
A J Culyer , A K Maynard, J W Posnett. "Reforming health care: an
introduction to the economic issues", in A. J. Culyer, A. K. Maynard and
J. W. Posnett (eds.) Competition in Health Care: Reforming the NHS, London: Macmillan,
1990, 1-11.
131.
A J Culyer. "Funding the future", in The White Paper and Beyond: One Year On,
(eds. E. J. Beck and S. A. Adam), Oxford: Oxford University Press
(Oxford Medical Publications), 1990, 58-69.
132.
A J Culyer. "Incentivos: para qué? Para quién?
De qué tipo?", in Associatión de Economia de la Salud, Reforma Sanitaria e Incentivos, Assoc.
de Econ. de la Salud, Barcelona, 1990, 39-53.
133.
A J Culyer. "The promise of a reformed
NHS: an economists angle", British
Medical Journal, 302, 1991,
1253-1256. (reprinted
in Professional Judgment and Decision
Making, Offprints (4), Milton
Keynes, Open University Press, 1992, 19-22).
134.
A J Culyer. "The normative economics of
health care finance and provision", in A. McGuire, P. Fenn and K. Mayhew
(eds.) Providing Health Care: the Economics
of Alternative Systems of Finance and Delivery, Oxford:
Oxford University Press, 1991, 65-98 (reprint with changes of 1989 article in Oxford
Review of Economic Policy).
135.
A J Culyer. "Conflicts between equity
concepts and efficiency in health: a diagrammatic approach", Osaka Economic Papers, 1991, 40: 141-154. (Reprinted in A. M. El-Agraa
(ed.) Public and International Economics,
New York: St Martins Press, 42-58).
136.
A J Culyer. "Egéazségügyi
szolgáltatások a vegyes gazdaságban", Esély, 91/3,
1991, 37-48 (reprint in Magyar of Health services in the mixed economy, in The Mixed Economy, 1982).
137.
A J Culyer. "Incentives: for what? For whom?
What Kind?", in G. Lopez-Casasnovas (ed.), Incentives in Health Systems, Berlin: Springer, 1991,
15-23 (reprint in English of article in Spanish in Reforma
Sanitaria e Incentivos, 1990),
138.
A J Culyer. "Reforming health services:
frameworks for the Swedish review", in A. J. Culyer (ed.) International Review of the Swedish Health
Care System, Studiefoerbundet Naeringsliv
och Saemhalle (Center for
Business and Policy Studies), Stockholm, 1991, 1-49.
139.
A J Culyer. "The promise of a reformed
NHS: an economists angle", in J. Dowie
(compiler) Professional Judgment and
Decision Making, Offprints (4), Milton Keynes: Open University Press, 1992,
19-22 (reprint of 1991 article in British Medical Journal).
140.
A J Culyer. "Hospital competition in the
UK: a (possibly) useful framework for the future" in R. B. Deber and G. G. Thompson (eds.), Restructuring Canadas Health Services System: How Do We Get There From
Here?, Toronto: University of Toronto Press, 1992, 317-330.
141.
A J Culyer. "The morality of efficiency in
health care - some uncomfortable implications", Health Economics, 1,
1992, 7-18. (Reprinted in A. King, T. Hyclak, S. McMahaon and R.
Thornton (eds.), North American Health
Care Policy in the 1990s, Chichester: Wiley,
1993, 1-24).
142.
A J Culyer, E van Doorslaer,
A Wagstaff. "Utilisation as a measure of equity
by Mooney, Hall, Donaldson and Gerard: Comment, Journal of Health Economics,
1992, 11: 93-98.
143.
A J Culyer. Need, greed and Mark Twain's cat,
in A. Corden, E. Robertson and K. Tolley
(eds.) Meeting Needs in an Affluent
Society, Aldershot: Avebury,
1992, 31-41.
144.
A J Culyer. "Sjukvård och sjukvårdsfinansiering
i Sverige" ("Health
care and health care financing in Sweden"), in A. J. Culyer et
al. Svensk Sjukyvård - Bäst i Världen? (Swedish Health Care -
the Best in the World?), Stockholm:
SNS Förlag, 1992, 9-31.
145.
A J Culyer. "Att
reformera sjukvärden:
ramar för den svenska genomgången"
("Reforming health services: Frameworks for the Swedish Review"), in
A. J. Culyer et al. Svensk Sjukyår
- Bäst i Världen? (Swedish
Health Care - the Best in the World?),
Stockholm: SNS Förlag, 1992, 32-65.
146.
A J Culyer. "Evaluation des technologies médicales: progrés des techniques et progrès de la science
économique", in J-R Moatti and C. Mawas (eds.), Evaluation des Innovations Technologiques et
Décisions en Santé Publiques, Paris: Coll. Analyse et Prospective, Eds
INSERM, 1992, 37-47.
147.
A J Culyer (with 34 others). The Appleton International
Conference: developing guidelines for decisions to forgo life-prolonging
medical treatment, Journal of Medical
Ethics, 1992, 18 (Supplement):
3.
148.
A J Culyer, E van Doorslaer,
A Wagstaff. "Access, utilisation and equity: a further comment, Journal of Health Economics,
1992, 11: 207-210.
149.
A J Culyer. "Health, health expenditures,
and equity", in E. van Doorslaer, A. Wagstaff
and F. Rutten (eds.) Equity in the Finance and Delivery of Health Care: an International
Perspective, Oxford: Oxford University Press (Oxford Medical Publications),
1993, 299-319,
150.
A J Culyer, A Meads.
"The United Kingdom:
effective, efficient, equitable?" Journal
of Health Politics, Policy and Law, 1993, 17: 667-688.
151.
A J Culyer. "Health care insurance and
provision", in N. Barr and D. Whynes (eds.) Current
Issues in the Economics of Welfare, Houndmills:
Macmillan, 1993, 153-175.
152.
A J Culyer. "The morality of efficiency in
health: some uncomfortable implications", in A. King, T. Hyclak, S. McMahon and R. Thornton (eds.) North American Health Care Policy in the
1990s, Chichester: Wiley, 1993, 1-24 (reprinted
from Health Economics, 1992).
153.
A J Culyer, A
Wagstaff. "QALYs versus HYEs", Journal of Health Economics,
1993, 12: 311-323.
154.
A J Culyer. "Conflicts between equity
concepts and efficiency in health: a diagrammatic approach", in A. M. El-Agraa (ed.) Public
and International Economics, New York, St Martin's Press, 1993, 42-58
(reprinted from Osaka Economic Papers,
1991).
155.
A J Culyer. "EI mercado interior: un medio
aceptable para conseguir un fin deseable", Hacienda Pública Española, 1993, 126: 39-49.
156.
A J Culyer, A
Wagstaff. "Equity and equality in
health and health care", Journal of Health Economics, 1993, 12:
431-457 (reprinted in N Barr (ed.) Economic
Theory and the Welfare State, Cheltenham: Edward
Elgar, 2001, 231-257 and in A J Culyer (Ed.) Health Economics: Critical Perspectives on
the World Economy, London:
Routledge, 2006, 483-509).
157.
A J Culyer, B Horisberger,
B Jonsson, F F F M Rutten.
"Introduction", European
Journal of Cancer, 1993, 29A, Suppl 7, S1-S2.
158.
A J Culyer, B. Jonsson.
"Ought cancer treatments to be immune from socio-economic evaluation? An
epilogue", European Journal of
Cancer, 1993, 29A, Supplement 7,
S31-S32.
159.
A J Culyer. "NHS reforms: a challenge or a
threat to NHS values?" The Health
Business Summary, No. 11, October 1994, 3-4.
160.
A J Culyer. "Finding answers to simple
questions", Parliamentary Brief,
1994, 3: 64.
161.
A J Culyer. "A proposal for a checklist of
reputable economics journals for the UK profession", Royal Economic Society Newsletter, 87, 1994, 16-17.
162.
A J Culyer. "The Culyer report (letter), The Lancet, 344, December 24/31, 1994, 1774.
163.
A J Culyer. "Economics and the incomplete
case for public support for research" (letter), Journal of the Royal College of Physicians of London, 29,
January/February 1995, 72.
164.
A J Culyer. "Cure at a cost", Times Higher Education Supplement,
(supplement, Synthesis: Medicine), January 20, 1995, i.
165.
A J Culyer. "Need: the idea won't do - but
we still need it", (Editorial) Social
Science and Medicine, 1995, 40:
727-730.
166.
A J Culyer. "Supporting research and
development in the NHS - Key points from the Culyer Report ", Refocus, 1995, Winter:
4-5.
167.
A J Culyer. "Supporting research and
development in the National Health Service", Journal of the Royal College of Physicians of London, 1995, 29: 216-224.
168.
A J Culyer. "Supporting R&D in the NHS
- some unresolved issues" in House of Lords, Minutes of Evidence Taken Before the Select Committee on Science and
Technology, HL Paper 12-iv, London: HMSO, 1995, 168-176.
169.
A J Culyer. Evidence before House of Lords
Select Committee on Science & Technology, Minutes of Evidence Taken before the Select Committee on Science and
Technology, HL Paper 12-iv, London: HMSO, 1995, 183-195 (passim)
170.
A J Culyer, A
Wagstaff. "QALYs versus HYEs: A
reply to Gafni, Birch and Mehrez",
Journal of
Health Economics, 1995, 14: 39-45.
171.
A J Culyer. "Preface: all is a flux yet
all is the same!", in International
Developments in Health Care, ed. Roger Williams, London, Royal College of
Physicians, 1995, vii-x.
172.
A J Culyer. "Chisels or screwdrivers? A
critique of the NERA proposals for the reform of the NHS", in A. Towse
(ed.) Financing Health Care in the UK: A
Discussion of NERA's Prototype Model to Replace the NHS, London: Office of
Health Economics, 1995, 23-37.
173.
A J Culyer. "Taking advantage of the new
environment for research and development" in M. Baker and S. Kirk (eds.) Research and Development for the NHS:
Evidence. Evaluation and Effectiveness, Oxford: Radcliffe Medical Press, 1995, 37-49
(reprinted with changes in Baker and Kirk 1998).
174.
A J Culyer. "Fundamentals for promoting
health gain efficiently and equitably in Northern Ireland: some reactions to
the Consultation Document Regional Strategy for Health and Social W11being,
1997-2002", in Northern Ireland Economic Council, Health and Personal Social Services to the Millennium, Belfast,
NIEC, 1995, 45-65.
175.
A J Culyer. "The NHS reforms - a challenge
or a threat to NHS values?" in A. J. Culyer and Adam Wagstaff (eds.) Reforming Health Care Systems: Experiments
with the NHS, Cheltenham: Edward Elgar, 1996, 1-14.
176.
A J Culyer, R G Evans. "Mark Pauly on welfare
economics: normative rabbits from positive hats", Journal of Health Economics,
1996, 15: 243-251 (reprinted in A J
Culyer (Ed.) Health Economics: Critical
Perspectives on the World Economy, London:
Routledge, 2006, 148-157).
177.
A J Culyer. "A personal perspective on
progress in research and development", in K. Aspinall
(ed.) The York Symposium on Health,
University of York, York, 1996, 33-44.
178.
A J Culyer. "The principal objective of
the NHS ought to be to maximise the aggregate
improvement in the health status of the whole community", British Medical Journal, 314, 667-669, 1997. (Reprinted with
changes in B. New (ed.), Rationing: Talk
and Action, London:
Kings Fund and BMJ, 1997, 95-100.
179.
A J Culyer. "0 impacta da economia da
saude nas politicas publicas", Nota
Economicas, 1997, 7: 38-48.
180.
A J Culyer. "Maximising
the health of the whole community: the case for", in B. New (ed.), Rationing: Talk and Action, London: Kings Fund and
BMJ, 1997, 95-100. (reprint with changes of BMJ 1997
article).
181.
A J Culyer. "A rejoinder to John
Harris", in B. New (ed.), Rationing:
Talk and Action, London:
Kings Fund and BMJ, 1997, 106-107.
182.
A J Culyer. Altruism and economics, in A. Nordgren and C-G. Westrim (eds.),
Altruism, Society, Health Care, Acta Universitatis Upsaliensis, Uppsala,
1998, 51-66.
183.
A J Culyer. Health and welfare resources at
the University of
York, Health-Care Focus, February 1998, 13-14.
184.
A J Culyer. Need - is a consensus possible? Journal of Medical Ethics, 1998, 24: 77-80 (Guest Editorial).
185.
A J Culyer. Foreword, in M. Baker and S. Kirk
(eds.) Research and Development for the
NHS, Abingdon: Radcliffe Medical Press, 1998, vi-x.
186.
A J Culyer. Taking advantage of the new
environment for research and development in Baker and Kirk (eds.), Research and Development for the NHS,
Abingdon: Radcliffe Medical Press, 1998, 53-66.
(reprint with changes of 1996 edition).
187.
A J Culyer. How could anyone imagine R&Ds
trial test is better patient care?, Health Services Journal, 9 April 1998, 18 (letter).
188.
A J Culyer. The NHS - an assessment, in L
Mackay, K Soothill and K Melia
(eds.), Classic Texts in Health Care,
Oxford, Butterworth Heinemann, 1998,
316-321 (Reprint of chapter 11 from Need
and the National Health Service, 1976).
189.
A J Culyer. How ought health economists to
treat value judgments in their analyses?, in M L Barer, T E Getzen and G L Stoddart (eds) Health, Health
Care and Health Economics, Chichester, Wiley,
1998, 363-371.
190.
A J Culyer. An input-outcome paradigm for NHS
research in forensic mental health, Criminal
Behaviour and Mental Health, 1999, 9:
355-371.
191.
A J Culyer. Economics and public policy: research and development as a public good in
P C Smith (ed.) Reforming Markets in
Health Care: An Economic Perspective, Buckingham,
Open University Press, 2000, 117-137.
192.
A J Culyer, A
Wagstaff. "Equity and equality in health and health care", in N Barr
(ed.) Economic Theory and the Welfare
State, Edward Elgar, Cheltenham, 2000. (Reprinted from Journal of Health Economics,
1993, 12: 431-457.)
193.
A J Culyer. Economics and ethics in health
care (editorial), Journal of Medical
Ethics, 2001, 27: 2001: 217-222.
194.
A J Culyer. Equity - some theory and its
policy implications, Journal of Medical
Ethics, 2001, 27: 275-283.
195.
A J Culyer. Values, policy impact and the
credibility of health economists, in W R Swan and P Taylor (eds.) Forward
to Basics: Promoting Efficiency While Preserving Equity (Proceedings of the
7th Canadian Conference on Health Economics, CHERA/ACRES, Carleton University,
Ottawa, 2001, 37-47.
196.
A J Culyer. Introduction: Ought NICE to have a
cost-effectiveness threshold?, in A Towse, C Pritchard and N Devlin (eds.) Cost-Effectiveness Thresholds Economic and
Ethical Issues, London, Office of Health Economics, 2002, 9-14.
197. A J Culyer,
R S Taylor, J Hutton. Developing the revised NICE
appraisal technical guidance to manufacturers and sponsors: opportunity or
threat? PharmacoEconomics,
2002, 20: 1031-1038.
198. A J Culyer,
M Rawlins. National Institute for Clinical Excellence and its value
judgements, British Medical Journal,
2004, 329: 224-227.
199.
A J Culyer, P
Littlejohns, G Leng, M Drummond. NICE
clinical guidelines: Maybe health economists should participate in guideline
development, British Medical Journal,
2004, 329: 571 (letter).
200.
A J Culyer, M
Rawlins. NICE and its value judgments: Authors' reply, British Medical Journal, 2004, 329: 741.
201.
A J Culyer, A Castelli. Rationing health care in Europe the United Kingdom, in J-Matthias Graf von der
Schulenburg and M Blanke (eds.) Rationing of Medical Services in Europe: An Empirical Study - A European Survey, Berlin:
IOS Press, 2004, 255-305.
202.
A
J Culyer. Involving stakeholders in healthcare decisions
the experience of the National Institute for Health and Clinical Excellence
(NICE) in England and Wales, Healthcare
Quarterly, 2005, 8: 56-60.
203.
G M Anderson, S E Bronskill, C A Mustard,
A J Culyer, D A Alter, D G Manuel. Both clinical
epidemiology and population health perspectives can define the role of health
care in reducing health disparities, Journal of
Clinical Epidemiology, 2005, 58:
757-762.
204.
C Godfrey, S Parrott, G Eaton, A J Culyer, C McDougall. Can we model the impact of increased drug
treatment expenditure on the U.K.
drug market? In Bjorn Lindgren and Michael Grossman
(eds.) Substance Use: Individual Behaviour, Social Interactions, Markets and
Politics, Vol. 36 in Advances in Health Economics and Health Services
Research, Amsterdam:
Elsevier, 2005, 257-275.
205.
A
J Culyer. Egészség-gazdaságtan, egészségügyi
közgazdászok, és az egészségpolitikai döntéshozás politikája (Health
economics, health economists and the politics of policy making). In László Gulácsi (Ed.) Egészég-Gazdaságtan,
Budapest: Medicina Könyvkiadó Rt, 2005, 35-44.
206.
A Szende, A J
Culyer. The inequity of informal payments for health care:
the case of Hungary, Health Policy,
2006, 75: 262-271.
207.
K Claxton, M Sculpher, A J Culyer, C McCabe, AH Briggs, R L Akehurst, M Buxton, J Brazier. Discounting and
cost-effectiveness in NICE - stepping back to sort out a confusion, Health Economics, 2006, 15: 1-4.
208. A J Culyer. NICE's use of cost-effectiveness as an
exemplar of a deliberative process, Health
Economics, Policy and Law, 2006, 1:
299-318.
209.
A J
Culyer. Paying for
performance: neither the end of the beginning nor the beginning of the end, HealthcarePapers,
2006, 6: 34-38.
210.
K Claxton, A J Culyer. Wickedness or folly? The ethics of NICEs decisions, Journal of Medical Ethics, 2006, 37: 373-378.
211.
A J
Culyer,
J Lomas. Deliberative processes and
evidence-informed decision-making in health care do they work and how might
we know? Evidence and Policy, 2006, 2: 357-371.
212.
A J Culyer.
Evidence, economics and values in coverage decisions, in Steve Morgan (Ed.) Toward a National Pharmaceuticals Strategy, Vancouver: Centre for
Health Services and Policy Research UBC, 2006, 10-11.
213.
A J
Culyer.
The bogus conflict between efficiency and equity, Health Economics, 2006, 15:
1155-1158 (Editorial).
214.
A J
Culyer,
R Saltman. Privatization assessing strategies in a
central Asian republic, in H. Zöllner, G. Stoddart and C. Selby Smith (Eds.) Learning to live with Health Economics, Copenhagen: WHO, 2006, III-95 - III-105
(copyrighted 2003, published 2006).
215. A J Culyer. Welfarism vs. Extra-Welfarism, Köz-Gazdaság Tudományos Füzetek (Public
Economics Science Journal) 2006, 1: 89-101.
216. A J Culyer.
"The nature of the commodity 'health care' and its efficient
allocation", in A J Culyer (Ed.) Health
Economics: Critical Perspectives on the World Economy, London: Routledge,
2006, 324-346 (reprinted from Oxford
Economic Papers, 1971, 23:
189-211).
217.
A J Culyer. "The normative economics of
health care finance and provision", in A J Culyer (Ed.) Health Economics: Critical Perspectives on
the World Economy, London: Routledge, 2006, 347-384, reprinted from A. McGuire, P. Fenn
and K. Mayhew (eds.) Providing Health
Care: The Economics of Alternative Systems of Finance and Delivery, Oxford:
Oxford University Press, 1991, 34-58).
218.
A J Culyer, A
Wagstaff. "Equity and equality in health and health care", in A J
Culyer (Ed.) Health Economics: Critical
Perspectives on the World Economy, London:
Routledge, 2006, 483-509, reprinted from Journal of Health Economics,
1993, 12: 431-457).
219.
A J Culyer, R G Evans. "Mark Pauly on
welfare economics: normative rabbits from positive hats", in A J Culyer
(Ed.) Health Economics: Critical
Perspectives on the World Economy, London:
Routledge, 2006, 148-157 (reprinted from Journal of Health Economics,
1996, 15: 243-251).
220.
A J Culyer.
Need - an instrumental view, in Richard Ashcroft, Angus Dawson, Heather
Draper and John McMillan (Eds.) Principles of Health Care Ethics, 2nd
Edition, Chichester: Wiley, 2007, 231-238.
221.
A J Culyer.
When and how cancer chemotherapy should be privately funded", Oncology
Exchange, 2007, 6: 47.
222.
A J Culyer,
C McCabe, A H Briggs, K Claxton, M Buxton,
R L Akehurst, M Sculpher, J Brazier.
Searching for a threshold, not setting one: the role of the National Institute
of Health and Clinical Excellence, Journal
of Health Service Research and Policy, 2007, 12: 56-58.
223.
A J
Culyer. Merit goods and the welfare economics of coercion in Wilfried Ver Eecke (Ed.) Anthology regarding Merit Goods. The Unfinished Ethical Revolution in
Economic Theory. West Lafayette: Purdue University
Press, 2007, 174-200 (reprinted from Public
Finance, 1971, 26: 546-572).
224.
K Claxton, A
J Culyer. Rights, responsibilities and NICE: A Rejoinder to Harris, Journal of Medical Ethics, 2007, 33:
462-464.
225. A J Culyer, C McCabe, A Briggs, K Claxton, M
Buxton, R Akehurst, M Sculpher, J Brazier
J. Not so
, Journal of Health
Services Research and Policy, 2007, 12:
190-191. (letter: reply to G Mooney, J Coast, S
Jan, D McIntyre, M Ryan and V Wiseman).
226.
A J Culyer.
NICE misconceptions, The Lancet, September 11 2007, on-line
at http://www.thelancet.com/journals/lancet/article/PIIS014067360761321X/comments
227. A J Culyer.
Equity of what in health care? Why the traditional answers don't help policy -
and what to do in the future, HealthcarePapers, 2007,
8(Sp): 12-26.
228. A J Culyer. Resource allocation in health care: Alan Williams decision maker, the authority and
Pareto, in A Mason & A Towse (eds.) The
Ideas and Influence of Alan Williams:
Be Reasonable Do it My Way! Oxford,
Radcliffe Publishing, 2007, 57-74.
229. L
S Robson, J Clarke, K Cullen, A Bielecky, C Severin, P Bigelow, E Irvin, A J Culyer,
Q Mahood. The effectiveness of occupational health and safety management
system interventions: a systematic review, Safety
Science, 2007, 45: 329-353.
230.
K Chalkidou, A
J Culyer, B Naidoo, P Littlejohns. Cost-effective public
health guidance: asking questions from the decision-maker's
viewpoint, Health Economics,
2008, 17: 441-448.
231.
K Claxton, A Briggs, M Buxton,
A J Culyer, C McCabe, S Walker, M J
Sculpher. Value based pricing for NHS
drugs: an opportunity not to be missed? British Medical Journal,
2008, 336: 251-254.
232.
W B F Brouwer, A J Culyer, N Job, A van Exel, F F H Rutten.
Welfarism vs. extra-welfarism, Journal of Health
Economics, 2008, 27: 325338.
233.
J Hurley, D Pasic, J Lavis, A J Culyer, C Mustard, W
Gnam. Parallel payers and preferred access: how Canadas Workers Compensation
Boards expedite care for injured and ill workers, HealthcarePapers,
2008, 8: 6-14.
234. J
Hurley, A J Culyer, W Gnam, J Lavis, C Mustard, D Pasic. Response to
commentaries, HealthcarePapers,
2008, 8: 52-54.
235.
K Chalkidou, T Walley, A J Culyer, P Littlejohns, A Hoy. Evidence-informed evidence-making, Journal of Health Services Research &
Policy, 2008, 13: 167-173.
236.
K
Claxton, A J Culyer. Not a NICE fallacy: A reply to
Dr Quigley, Journal of Medical Ethics,
2008, 34: 598-601.
237. A J Culyer, B Amick, A
LaPorte. What is a little more health and safety
worth? in E Tompa, A J Culyer, R Dolinschi (Eds.) Economic Evaluation of Interventions for Occupational
Health and safety: Developing Good Practice, Oxford: Oxford University Press, 2008, 15-35.
238. A J Culyer, M Sculpher. Lessons from health technology
assessment, in E Tompa, A J Culyer,
R Dolinschi (Eds.) Economic
Evaluation of Interventions for Occupational Health and safety: Developing Good
Practice, Oxford:
Oxford University Press, 2008, 51-69.
239. A J Culyer, E Tompa. Equity, in E Tompa,
A J Culyer, R Dolinschi. (Eds.) Economic Evaluation of Interventions for
Occupational Health and safety: Developing Good Practice, Oxford: Oxford University Press, 2008,
215-231.
240.
E Tompa, A J Culyer, R Dolinschi.
Suggestions for a reference case, in E Tompa, A J Culyer, R Dolinschi (Eds.) Economic Evaluation of Interventions for
Occupational Health and safety: Developing Good Practice, Oxford: Oxford University Press, 2008,
235-244.
241.
C McCabe, K Claxton, A J Culyer. The
NICE cost effectiveness threshold
what it is and what that means, PharmacoEconomics, 2008, 26: 733-744.
242.
K Chalkidou, A
J Culyer, P Littlejohns, P Doyle, A Hoy.
Imbalances in funding for clinical and public health research in the UK:
can NICE research recommendations make a difference? Evidence and Policy, 2008, 4: 355-369.
243.
J Hurley, D Pasic, J Lavis, C Mustard, A J Culyer, W Gnam.
Parallel lines do intersect: interactions between the workers compensation
and provincial publicly financed health care systems in Canada, HealthCare Policy, 2008, 3: 100-112.
244.
Chalkidou K, A J
Culyer, B Naidoo, P Littlejohns. "The challenges of developing
cost-effective public health guidance: a NICE perspective", in S Dawson
and Z S Morris (eds.) Future Public
Health: Burdens, Challenges and Opportunities, Basingstoke:
Palgrave Macmillan, 2009, 276-291.
245.
A J Culyer How
Nice is NICE? A Conversation with Anthony Culyer, Health Care Cost
Monitor, Hastings Centre Blog, 2009.
246.
Cookson R, A
J Culyer. Measuring overall
population health - the use and abuse of QALYs, in Killoran A, Kelly M (eds). Evidence Based Public Health: Effectiveness and Efficiency, Oxford:
Oxford University Press, 2010, 148-168.
247.
A J Culyer.
"Perspective and desire in comparative effectiveness research - the
relative unimportance of mere preferences, the central importance of
context", Pharmacoeconomics,
2010, 28: 889-897.
248.
K Claxton, M Paulden, H Gravelle, W Brouwer, A J Culyer. Discounting and decision
making in the economic evaluation of health-care technologies, Health Economics, 2011, 20: 2-15.
249.
R Chase, A J
Culyer, M Dobrow, P Coyte, C Sawka, S OReilly, K Laing, M Trudeau, S
Smith, J Hoch, S Morgan, S Peacock, R Abbott, T Sullivan. Access to Cancer
Drugs in Canada: Looking Beyond Coverage Decisions, Healthcare Policy, 2011, 6: 27-35.
250.
A J Culyer.
UK report: NHS reforms, Health Care
Cost Monitor, 2011, 1-2. The Hastings Centre, on-line at http://healthcarecostmonitor.thehastingscenter.org/anthonyculyer/u-k-report-nhs-reforms.
251.
P Tso, A
J Culyer, M Brouwers,
M J Dobrow. Developing a decision
aid to guide public sector health policy decisions: A study protocol, Implementation Science, 2011, 6: 46.
252.
A J Culyer. Hic sunt dracones: the future of Health Technology Assessment
one economists perspective, Medical
Decision Making, first
published on November
18, 2011 as doi:10.1177/0272989X11426483, forthcoming Jan/Feb 2012.
253.
A J Culyer, Y Bombard,
An equity framework for health technology assessments, Medical Decision Making, 0272989X11426484, first
published on November 7,
2011 as doi:10.1177/0272989X11426484,
forthcoming May/Jun 2012.
Reprinted articles
A J Culyer "The economics of health systems"
in The Price of Health, Melbourne:
Office of Health Care Finance, 1969, 36-62 (reprinted as ch.7 in J. R. G.
Butler and D. P. Doessel (eds.), Health Economics: Australian Readings, Sydney: Australian
Professional Publications, 1989, 145-66).
A J Culyer "The nature of the commodity
'health care' and its efficient allocation", Oxford Economic Papers, 1971,
23: 189-211 (reprinted as Ch. 2 in A. J. Culyer and M. H. Cooper (eds.), Health Economics, London: Penguin, 1973,
also in A J Culyer (Ed.) Health
Economics: Critical Perspectives on the World Economy, London: Routledge,
2006, 148-157).
A J Culyer "Merit goods and the welfare
economics of coercion", Public
Finance, 1971, 26: 546-72. (Reprinted in Wilfried Ver Eecke,
Merit Goods: The Birth of a New Concept. The Unfinished Ethical
Evolution in Economic Theory.
Ashland Ohio: Purdue University
Press, 2006, 174-200).
A J Culyer "Medical care and the
economics of giving", Economica, 1971, 38:
295-303 (reprinted as Ch. 18 in M. Ricketts (ed.), Neoclassical Microeconomics, Vol. 2, Aldershot:
Edward Elgar, 1989, pp. 310-18).
A J Culyer, A Williams and R J Lavers
"Social indicators: health", Social
Trends, 1971, 2:
31-42 (reprinted as Health indicators in Andrew Shonfield and Stella Shaw (eds.) Social Indicators and Social Policy, London: Heinemann, 1972).
A J Culyer The NHS - an assessment, in L
Mackay, K Soothill and K Melia
(eds.), Classic Texts in Health Care,
Oxford, Butterworth Heinemann, 1998,
316-321 (Reprint of chapter 11 from Need and
the National Health Service, 1976).
A J Culyer and Heather Simpson
"Externality models and health: a Rückblick over
the last twenty years", The Economic
Record, September 1980, 56: 222-30. (Reprinted with changes in P M Tatchell (ed).
Economics and Health: Proceedings of the
First Australian Conference of Health Economists, Canberra:
Australian National University
Press, 1980, 139-157).
A J Culyer
and A K Maynard "Cost-effectiveness of duodenal ulcer treatment", Social Science and Medicine, 15C, 3-11,
1981. (Reprinted in shortened form in Bernard S. Bloom (ed.), Cost-Benefit and Cost-Effectiveness Analysis
in Policymaking. Cimetidine as a Model, New York: Biomedical Information
Corporation, 1982, 128-31).
A J Culyer "Health services in the mixed
economy" in Lord Roll of Ipsden (ed.), The Mixed Economy, London, Macmillan,
1982, 128-144. (reprinted in Magyar as "Egeszsegugyi szolgaltatasok a vegyes gazdasagban", Esely, 9113,
1991, 37-48).
A J Culyer "The normative economics of
health care finance and provision", Oxford Review of Economic Policy, 5, 1, 1989,
34-58. (reprinted with changes in A. McGuire, P. Fenn and K. Mayhew (eds.) Providing Health Care: The Economics of
Alternative Systems of Finance and Delivery, Oxford: Oxford University
Press, 1991, 65-98, also in A J Culyer (Ed.) Health Economics: Critical Perspectives on the World Economy, London:
Routledge, 2006, 148-157).
A J Culyer "Conflicts between equity
concepts and efficiency in health: a diagrammatic approach", Osaka Economic Papers, 1991, 40: 141-154. (Reprinted in A. M. El-Agraa (ed.) Public and International Economics, New York: St Martins Press, 42-58).
A J Culyer "The promise of a reformed
NHS: an economists angle", British
Medical Journal, 302, 1991,
1253-1256. (reprinted
in Professional Judgment and Decision
Making, Offprints (4), Milton
Keynes, Open University Press, 1992, 19-22).
A J Culyer
"The morality of efficiency in health care - some uncomfortable
implications", Health Economics,
1992, 1: 7-18. (Reprinted in A. King, T. Hyclak,
S. McMahaon and R. Thornton (eds.), North American Health Care Policy in the 1990s, Chichester: Wiley, 1993, 1-24).
A J Culyer and A Wagstaff "Equity and
equality in health and health care", Journal of Health Economics,
1993, 12: 431-457 (reprinted in N Barr (ed.) Economic Theory and the Welfare State, Cheltenham: Edward Elgar, 2001, 231-257 and in A J Culyer (Ed.) Health Economics: Critical Perspectives on
the World Economy, London: Routledge, 2006,
483-509).
A J Culyer "Taking advantage of the new
environment for research and development" in M. Baker and S. Kirk (eds.) Research and Development for the NHS:
Evidence. Evaluation and Effectiveness, Oxford: Radcliffe Medical Press, 1995, 37-49
(reprinted with changes in Baker and Kirk Baker and Kirk (eds.), Research and Development for the NHS,
Abingdon: Radcliffe Medical Press, 1998, 53-66.
A J Culyer and R G Evans "Mark Pauly on
welfare economics: normative rabbits from positive hats", Journal of Health Economics,
1996, 15: 243-251 (reprinted in A J Culyer (Ed.) Health Economics: Critical Perspectives on the World Economy, London: Routledge, 2006, 148-157).
A J Culyer "The principal objective of
the NHS ought to be to maximise the aggregate
improvement in the health status of the whole community", British Medical Journal, 314, 667-669, 1997. (Reprinted
with changes in B. New (ed.), Rationing:
Talk and Action, London:
Kings Fund and BMJ, 1997, 95-100).
B.
Books
1. A J Culyer,
F M M Lewes and G Brady, The Holiday Industry of Devon and Cornwall,
London, HMSO,
1970, pp. x + 263.
2. M H Cooper and A J Culyer (eds.) Health
Economics, London,
Penguin Books, 1973, pp. 396.
3. A J Culyer, The Economics of Social Policy, Martin
Robertson, London,
1973 (Japanese ed. 1976), xii + 268.
4. A J Culyer and
F W Paish (eds.) Benham's Economics, Pitman, London, 1973, pp. xiv + 562.
5. A J Culyer
(ed.) Economic Policies and Social Goals:
Aspects of Public Choice, London:
Martin Robertson, 1974, pp. vii + 349.
6. A J Culyer, Need and the National Health
Service: Economics and Social Choice, London, Martin Robertson, 1976, pp. xii +
163 [chapter 11 reprinted as ch. 55 in Classic Texts in Health Care, 1998, eds. Mackay, Soothill & Melia]
7. A J Culyer,
J Wiseman and A Walker (eds.) An Annotated Bibliography of Health
Economics, London, Martin Robertson, 1977, pp. xvii + 361.
8. A J Culyer and
V Halberstadt (eds.) Human Resources and Public Finance, Paris: Cujas,
1977, pp. viii + 309.
9. A J Culyer
and K G Wright (eds.) Economic Aspects of
Health Services, London: Martin Robertson, London, 1978, pp. ix +
190.
10. A J Culyer, Measuring Health: Lessons for Ontario, Toronto, University
of Toronto Press for the
Ontario Economic Council, 1978, pp. vii + 189.
11. A J Culyer, The Political Economy of Social
Policy, Oxford, Martin Robertson,
1980 (revised edition 1983), pp. xii + 340 (reprinted by Gregg Revivals, 1991).
12. A J Culyer
(ed.) Health Indicators: An International Study for the European Science Foundation,
London: Martin Robertson, 1983 (also New York: St. Martin's
Press, 1983), pp. xii + 223.
13.
A J Culyer and B Horisberger
(eds.) Economic and Medical Evaluation of Health Care
Technologies, Heidelberg: Springer, 1983 (trans. as: Technologie in
Gesundheitswesen: Medizinische und Wirtschaftliche Aspekte, Heidelberg: Springer, 1984), pp. xxvi + 405.
14. A J Culyer, Economics,
Oxford: Basil
Blackwell, 1985, pp. xxii + 737.
15. A J Culyer and
G Terny (eds.) Public
Finance and Social Policy, Detroit:
Wayne State UP, 1985, pp. xviii + 370.
16. A J Culyer, C Blades, J Wiseman and A Walker
(compilers) The International Bibliography of Health Economics (2 vols.), Brighton: Wheatsheaf, 1986,
vol. 1, pp. xviii + 658; vol. 2, pp. xiv + 434.
17. A J Culyer and
B Jonsson (eds.) Public
and Private Health Services: Complementarities and Conflicts, Oxford: Basil Blackwell,
1986, pp. vii + 242.
18. A J Culyer, Health Care Expenditures in Canada:
Myth and Reality; Past and Future, Canadian Tax Paper No. 82, Toronto:
Canadian Tax Foundation, 1988, pp. ix + 110,
19. A J Culyer (ed.)
Standards for Socioeconomic Evaluation of
Health Care Products and Services, Heidelberg:
Springer, 1990, pp. xi + 184.
20. A J Culyer A
K Maynard and J W Posnett (eds.) Competition in Health Care: Reforming the NHS, London: Macmillan, 1990, pp. vii + 255.
21. A J Culyer, The Economics of Health, Aldershot: Edward
Elgar, 1991, 2 vols., pp. xiii +
402; pp. xiii + 407.
22. A J Culyer, The Political Economy of Social Policy, Aldershot:
Gregg Revivals, 1991, pp. xiii + 340 (reprint of 1983 book).
23. A J Culyer,
M L Barer and G Mooney (eds.) Some Recent Developments in Health Economics,
published as vol. 34, No. 9 of Social Science and Medicine, 1992, pp. 123.
24. A J Culyer,
R G Evans, J-M von der Schulenburg, W P M M van de Ven and B A Weisbrod Svensk Sjukyård: Bäst i Världen?
(Swedish Health Care: Best in the World?), Stockholm: SNS Förlag,
1992, ISBN 91-7150-430-3, pp. 211. (translation of two
1991 reports listed in section C).
25. A J Culyer and
A Wagstaff (eds.) Reforming Health Care
Systems: Experiments with the NHS, Cheltenham:
Edward Elgar, 1996, pp. xii + 177.
26. A J Culyer and
A Maynard (eds.) Being Reasonable about
the Economics of Health: Selected Essays by Alan
Williams, Cheltenham: Edward Elgar, 1997, pp. xvi + 371.
27. A J Culyer and
J P Newhouse (eds.) Handbook of Health
Economics, Vols 1A and 1B, Amsterdam, North Holland, 2000 (Vol. 1A, pp. xxiii + 890 + 86, Vol.
1B, pp. xxvi + 1,910 + 86).
28. A J Culyer, The Dictionary of Health Economics, Cheltenham:
Edward Elgar, 2005, pp. xiv + 390.
29. A J Culyer, (Ed.) Health Economics: Critical
Perspectives on the World Economy, 4 Vols., Abingdon: Routledge,
2006, Vol. 1, pp. xxvi + 545; Vol. 2, pp,. xi + 450;
Vol. 3, pp. viii + 386; Vol. 4, pp. xi + 600.
30. E Tompa, A J Culyer, R Dolinschi (Eds.) Economic
Evaluation of Interventions for Occupational Health and safety: Developing Good
Practice, Oxford:
Oxford University Press, 2008, pp. xvi + 295.
31. A J Culyer, The Dictionary of Health Economics, 2nd
edition, Cheltenham: Edward Elgar, 2010.
C.
Monographs, Pamphlets, Occasional Papers and Discussion Papers
1. F. M. M. Lewes, A J Culyer and G A Brady, The Transport of Holiday makers in Devon and
Cornwall, Exeter: University of Exeter, 1966, pp. 63.
2. M H Cooper and A J Culyer, The Price of Blood, London: Institute of
Economic Affairs, 1968, pp. 47.
3. A T Peacock and A J Culyer, Economic Aspects
of Student Unrest, London: Institute of Economic Affairs, 1969, pp. 23.
4. M H Cooper and A J Culyer, The
Pharmaceutical Industry, London: Dun and Bradstreet and Economists'
Advisory Group, 1973, pp. xvi + 43.
5. A J Culyer
and A K Maynard, Some Major Issues in Health Policy, Dublin: National Economic and
Social Council, 1977, pp. 94.
6. A J
Culyer, Expenditure on Real Services:
Health, Milton Keynes: Open University Press, 1979, pp. 59.
7. A J Culyer
and M H Cooper, The Economics of Universities, Dunedin:
University of Otago Discussion Paper 8103.
8. A J Culyer, The Withering of the Welfare State? 1985 E.
S. Woodward Lectures, Vancouver: University of British Columbia, 1986, pp. 41.
9.
A J Culyer, Whither the Welfare State? 1985 E. S. Woodward Lectures, Vancouver:
University of British Columbia, 1986, pp. 41.
10. A J Culyer, Health Service Ills: the Wrong Economic
Medicine, York: Centre for Health Economics, University of York, 1986,
Discussion Paper 16, pp. 30.
11. A J Culyer,
C Donaldson and K Gerard, Alternatives
for Funding Health Services in the U.K., London: Institute of Health
Services Management, Working Paper No. 2, 1988, pp. 26.
12. A J Culyer,
C Donaldson and K Gerard Financial
Aspects of Health Services: Drawing on Experience, London: Institute of
Health Services Management, Working Paper No. 3, 1988, pp. 73.
13. A J Culyer
and J Brazier, Alternatives for Organising the Provision of Health Services in the U.K.,
London: Institute of Health Services
Management, Working Paper No. 4, 1988, pp. 30.
14. A J Culyer,
J. Brazier and 0. O'Donnell, Organising Health Service Provision: Drawing on Experience,
London: Institute of Health Services Management, Working Paper No. 5, 1988, pp.
76,
15. A J Culyer (with
others under the Chairmanship of Barbara S. Young Working Party on Alternative Delivery and Funding of Health Services:
Final Report,), London: Institute of Health Services Management, 1988, pp.
54.
16. A J Culyer and
A Mills, (eds.) Perspectives on the Future of Health Care in Europe, York: Centre for
Health Economics, 1989, Occasional paper, pp. ii + 150.
17. A J Culyer, Cost-containment in Europe, York: Centre
for Health economics, University of York, 1989, Discussion Paper 62, pp. 42.
18. A J Culyer, Competition and Markets in Health Care: What
we Know and What we Don't, York: Centre for Health
Economics, University of York, 1989, NHS White Paper Occasional Paper 3, pp.
29.
19. A J Culyer, The Internal Market: An Acceptable Means to
a Desirable End, York: Centre for Health Economics, University of York,
1990, Discussion Paper 67, pp. 25.
20. A J Culyer, Ethics and Efficiency in Health Care: Some
Plain Economic Truths, York: Centre for Health Economics and Policy
Analysis, McMaster University, Canada, 1991, Health
Policy Commentary Series C91-1, pp. 27.
21. A J Culyer, Health, Health Expenditures and Equity,
York: Centre for Health Economics, University of York, 1991, Discussion Paper
83, pp. 34.
22. A J Culyer
and A Wagstaff, Need.
Equality and Social Justice, York: Centre for Health Economics, University
of York, 1991, Discussion Paper 90, pp. 16; also in Report No 92.14 of
Institute for Medical Technology Assessment, Erasmus
University, Rotterdam, 1992.
23. A J Culyer, Health Care and Health Care Finance in
Sweden: The crisis that never was, the tensions that ever will be (and how to
ease them), Stockholm: Studiefoerbundet Naeringsliv och Sarnhaelle (Center for Business and Policy Studies),
Occasional Paper 33, 1991, pp. 30 (Published in Swedish as Svensk
Sjukvård - Bäst i Världen?, Stockholm, SNS,
1992).
24. A J Culyer, International Review of the Swedish Health
Care System, (ed.), Stockholm: Studiefoerbundet Naeringsliv och Sarnhaelle (Center for
Business and Policy Studies), Occasional Paper 34, 1991, pp. 198 (Published in
Swedish in Sjukvård - Bäst i Världen?, Stockholm, SNS 19921
25. A J Culyer, Need, Equity and Equality in Health and
Health Care, York: Centre for Health Economics, University of York, 1992,
Discussion Paper 95, pp. 29 (with Adam Wagstaff);
also in Report No 92.14 of Institute for Medical Technology Assessment, Erasmus
University, Rotterdam, 1992.
26. A J Culyer, Equity in Health Care Policy, Toronto: Premier's
Council on Health, Well-Being and Social Justice, 1992, pp. 31.
27. A J Culyer
with other members of the Committee, Special
Health Authorities: Research Review, a Report by the Review Advisory Committee
(The Thompson Report), London: HMSO, pp. 56, 1993.
28. A J Culyer, Supporting Research and Development in the
NHS, a Report to the Minister of Health by a Research and Development Task
Force chaired by A. J. Culyer, London: HMSO, 1994, pp. 85.
29. A J Culyer, Funding Research in the NHS, York:
Centre for Health Economics, University of York, Discussion Paper 125, 1994,
pp. 30.
30. A J Culyer, Equality of What in Health
Policy: Conflicts Between the Contenders, York: Centre for Health
Economics, University of York, Discussion Paper 142, 1995, pp. 21.
31. A J Culyer,
J-M. Graf von der Schulenburg and W.
P. M. M. van de Ven, Swedish Health Care Revisited, Stockholm: SNS, Occasional Paper
71, 1995, pp. 26.
32. A J Culyer, Economics and Public Policy - NHS Research
and Development as a Public Good, York: Centre for Health Economics,
Discussion Paper 163 (The York Series on the NHS White Paper - A Research
Agenda), 1999, pp21.
33. Godfrey,
C., Eaton, G., McDougall, C. and A. J.
Culyer, The Economic and
Social Costs of Class A Drug Use in England and Wales, 2000, London: Home Office Research Study
249, Home Office Research, Development and Statistics Directorate, 2002 (pp.
62).
34. A J Culyer, Eaton,
G., Godfrey, C., Koutsolioutsos, H., and McDougall,
C. Economic and Social Cost of Substance Misuse in the United Kingdom
Review of the methodological and empirical studies of the economic and social
costs of illicit drugs, (a report to the Home Office), York: University of York and Home
Office, Centre for Criminal Justice Economics & Psychology, Research Series
Report 03-01, 2002 (pp. 117).
35. L Robson, J Clarke, K Cullen, A Bielecky, C Severin, P Bigelow, E
Irvine, A J Culyer and Q Mahood The Effectiveness of Occupational Health
and safety Management Systems: A Systematic Review (Full Report), Toronto:
Institute for Work & Health, 2005, pp.153.
36. L Robson, J Clarke, K Cullen, A Bielecky, C Severin, P Bigelow, E
Irvine, A J Culyer and Q Mahood The Effectiveness
of Occupational Health and safety Management Systems: A Systematic Review
(Summary), Toronto: Institute for Work & Health, 2005.
37. J. Lomas, A J Culyer, C. McCutcheon, L. McAuley,
and S Law (2005), Conceptualizing and
Combining Evidence for Health System Guidance. Ottawa: Canadian Health
Services Research Foundation, 2005, pp.38.
38. A J
Culyer, Weighing up the
evidence: making evidence-informed guidance accurate, achievable, and
acceptable, (Convenor with Jonathan Lomas) 2006, Ottawa:
Canadian Health Services Research Foundation, 14 pp.
39. A J
Culyer, Review of Citizens
Councils and Recommendations for the Creation of a Citizens Council in Ontario
as Mandated under the Transparent Drug System for Patients Act,
University of Toronto Priority Setting in Health Care Research Group (with
Andreas Laupacis, Doug Martin, Alan Hudson, Wendy
Levinson, Terrence Sullivan,
Bill Evans, Steven Pearson, Irfan Dhalla,
Tasha Jeyanathan)
2006.
40. K Claxton, Mark Sculpher and A J
Culyer, Mark versus Luke?
Appropriate methods for the evaluation of public health interventions, University
of York: Centre for Health Economics Research Paper RP31, 2007.
41. A J Culyer. Deliberative
Processes in Decisions about Health Care Technologies: Combining Different
Types of Evidence, Values, Algorithms and People, London: Office of
Health Economics, 2009, pp. 1-20.
42. A J Culyer. Health, distribution and fairness sorting out the theory and matching
it to future policy practice (notes for the Select Committee on Health),
House of Commons Select Committee on Health, 3rd Report: Health
Inequalities, Vol. 2, 2009.
43.
M. J. Dobrow, R.
Chafe, H. E. D. Burchett, A J Culyer,
L. Lemieux-Charles Designing Deliberative
Methods for Combining Heterogeneous Evidence: A Systematic Review and
Qualitative Scan. A Report to the Canadian Health Services Research Foundation, Ottawa: Canadian Health Services Research
Foundation, 2009, pp. 24 + 30.
44. A J Culyer, Y. Bombard. An equity checklist: a
framework for health technology assessments, CHE Research Paper 62, York: Centre for Health
Economics, 2011.
45.
Adam Wagstaff and A J Culyer Four decades of Health Economics through a bibliometric
lens, World Bank Policy Research Working Paper
Series, 5829, 2011.
 Return
to index
Return
to index
Current articles
Hic
sunt dracones: The future
of Health Technology Assessment one economists perspective
Anthony
J Culyer
University of Toronto (Canada) and University of York (England)
All
effective treatment must be free
Here be dragons may not have actually
appeared on any known early map of the world but it is on the Lenox Globe of
1510 in the New York Public Library, and monsters, giant horned men, and other
similarly terrifying beasts were certainly sketched in early maps of the
remoter and mostly unexplored regions of the world. One may draw an analogy
between such maps and the current state of Health Technology Assessment (HTA).
There is a large terrain of well-researched and largely well-understood methodseconomic,
biostatistical, and epidemiologicalon which most researchers are engaged in
what is aptly called normal science (Kuhn 1972). There are many important
research topics, both applied and methodological, that customarily fill the
pages of journals such as this and that are also normal in the Kuhnian sense
of operating within the conventional optimising paradigm of most
cost-effectiveness analysis as illustrated by Drummond et al. (2005) and Gold
et al. (1996), and many others. I do not intend to dwell here on research
falling into this category. Nor do I intend, however, to devalue it by implying
that it is somehow unadventurous or merely conventional. On the contrary, HTA is a living example of
the intense creativity that is possible within a paradigm, and HTA is not at
all normal in respect of the amazing bridging that has taken place across
conventional disciplinary (and faculty) lines, between clinical, statistical,
and philosophical disciplines as well as social sciences, and it seems to me a
considerable and highly unusual achievement that there should be so little
misunderstanding between these disciplines. Indeed, an eavesdropper on a
conversation between its practitioners would be hard-pressed to tell from
language alone whether a speaker was an epidemiologist, a statistician, a
clinician, an ethicist or an economist. This is what I imagine people may have
in mind in making a distinction between multidisciplinarity
and interdisciplinarity.
Fascinating though such an interdisciplinary
story would be, that is not what I want to draw to
your attention. My concerns about HTA relate to the fact that, when applied, it
inevitably has a political context. It is political both with a large P and a
small one. The large P relates to the political ideology of health services
and springs from the notion of a public interest element of health services.
This is an interest that can be cast in many languages for, example, in
political language, solidarity; or, in Marxian language, from each according to their ability; to
each according to their need; or, in neoclassical economic language, public
goods and caring externalities. It
finds particular expression in the idea, which I think can be first attributed
to Archie Cochrane (Cochrane 1972), that the only health care warranting public
financing or public delivery is health care that is demonstrably effective.
Cochranes slogan, which I have stolen as the sidehead
for this section, was All effective treatment must be free (Cochrane 1972).
It is, of course, perfectly possible to argue that it would be a rather good
marketing strategy for any private health insurance agency to claim that the
only services it would cover would be those in which one could have confidence
that they were truly effective, even cost-effective, for there must be a
substantial fraction of any population for whom that would be an attractive
bundle to purchase, whether privately or through taxes, since there seems
little point, at least from a consumers point of view, in having to purchase
services of no value. Fascinating though
this tack would be, like the interdisciplinary story I shall set it aside in
order to dwell on the small p political context. This is the context in which
the political creator of NICE, Frank Dobson, when asked as Secretary of State
for Health whether he thought it would work, said probably not, but its worth
a bloody good try. Applied HTA is political both in the sense that it
inherently embodies value judgments, including ones about equity, or fairness,
and in the sense that the identification and acceptance of value judgments of
any kind requires a process within the body politic, one, moreover, that needs
to have particular characteristics if it is to lead to acceptable decisions.
An
economists angle
I ought to make plain the purpose of HTA and
the key questions that it addresses or ought to address. HTA exists to help
public decision makers make evidence-informed choices at the level at which
formulary, insurance coverage, and clinical guideline decisions are taken so as
to advance the publics health. HTA ought to be seen as an aid to thought;
never a substitute for it. It is a tool and, as such, ought to be useful,
credible and fit for purpose. It is not a chisel to be used as a screwdriver,
nor a screwdriver to be used as a chisel. It should reveal what we do not know
as well as what we do, what sort of confidence we may have in the available
information, and be capable of indicating what other kinds of information would
further aid decision makers. It ought to help decision makers integrate
different kinds of information and expose the values that ought to underpin all
such decisions. Regarding key questions, the main ones are very familiar: does
an intervention (or health technology) work? For whom does it work? How well does it work?
Relative to what alternatives? At what cost? Is it
worthwhile? Can it be introduced (or withdrawn) and used in fair
ways? What values are embodied in the answers to the foregoing? And what
is the legitimate source of those values?
Even though many other disciplines provide
crucial inputs, especially empirical inputs, to answer these
question, it is economics that has provided the overall analytical
framework for Comparative Effectiveness Research (CER) and Cost-Effectiveness
Analysis (CEA) in HTA. Economics has specifically prescribed
a broadly utilitarian type of optimization (constrained maximization), though
the stipulation of health rather than utility as the maximand is a
significant departure from utilitarianism as normally practised. HTAs long-standing concern over the way in
which this maximand is distributed over a jurisdictions population is another
departure, such distributional concerns being of sublime indifference to strict
utilitarians. Economics has also specified the general character of the
evidence required to determine probable cost-effectiveness (clinical of course,
but also other evidence, especially that related to costs, non-clinical
outcomes and outcomes affecting third parties). It is economists who insist on
the separate roles of science and social value judgments and who have
emphasized that what qualifies one to make judgments about the former rarely
also qualifies one to make judgments about the latter. Economics has introduced
the HTA world to some of its own vocabulary, which has been quickly understood
and absorbed into the conventional practice of HTA: words (and the inevitable
acronyms) like incremental cost-effectiveness
ratio (ICER); publicness, in the sense of a benefit whose enjoyment by one
person does not diminish enjoyment for another; opportunity cost, in the
sense of the most highly valued alternative use of the resources undergoing
investigation; social welfare function (SWF), in the sense of how the
satisfied preferences of many individuals are linked or added up;
externality, in the sense of the impact on others of ones behaviour. Economics has also brought some of its own
techniques to the table: Quality-adjusted Life-years (QALYs) and other outcome
concepts; discrete choice experiments (DCE) and other experimental methods
(many in association with cognitive psychology); time preference and
discounting. Indeed, it would be a challenge to find any method in use today
that remains uniquely the property of any one discipline, including economics.
A short list of such core disciplines ought to include anthropology,
biostatistics, cognitive psychology, decision theory, epidemiology, ethics,
ethnography, management, mathematics, political science, public administration,
qualitative research, and social policy.
Despite this rich multi-disciplinary input,
it remains the case that the current guidance, whether from institutions like
NICE and OHTAC or academic textbooks and articles, fails to deal with equity,
in the sense of fairness, with anything like adequacy. This brings me to the
dragons that I think need slaying which, like sleeping dogs, have
been left to lie but which, if aroused, are capable of more mischief and
destruction than any dog.
Two
dragons
The first dragon is equity and, in
particular, how one may embody equity considerations into HTA. By equity I
mean interpersonal fairness in the receipt of health care and the distribution
of its consequences. Economists have a well-developed corpus of theory, both
for describing the characteristics of a first-best allocation of resources to
production and the fruits of that production to final consumers. They also have
a well-developed set of principles for putting that analysis to work in a
second-best world. Complementing those principles is an impressive array of
empirical tools. It is all adaptable to the circumstances of the public sector
as well as the private. And it has been, moreover, adapted to the circumstances
of health care and health.
What economists have never been able
satisfactorily to do is develop any analysis of equity of comparable
sophistication, comparable applicability and comparable mutual agreement. Nor,
alas, has the vacuum been filled by anyone else, though Johri
and Norheims review (2009) is a useful beginning.
The consequence is that the committees that make recommendations about the
adoption and funding of new health care interventions, or disinvestment in old ones, do not know how to address matters of equity. Nor do
they know how to integrate such considerations into efficiency analyses.
Economists are strong on what not to
do. Do not identify equity with equality, nor health
with welfare, nor need with priority. Do not assume that equity trumps
efficiency, nor that efficiency trumps equity. The
list may readily be prolonged. The trouble is that these prohibitions are
nearly always what people do tend to
ignore That is not surprising given that economists, along with ethicists and
other social analysts, have failed to stipulate what it is that one do instead.
By the same token, the aforesaid failure has, again not surprisingly, left an
empirical void which stands in marked contrast to the evidential base that
exists for efficiency studies, so that even if we suddenly knew what it is that
we should do with respect to equity, we would hardly be able, as a practical
matter, to do it. As it happens, I think there is a solution that will banish
this dragon to even further reaches of our known landscape, but before
revealing this I must turn to the second dragon.
The second dragon is associated with the
first and, unless this dragon is also slain, or at least banished, it will make
it mightily difficult to dispose of dragon number one. Dragon number two is our
ignorance as to the character of a process that might enable us to integrate
equity in HTA. Specifically, the challenge
is that we are short of an adequate understanding of the processes necessary for combining different
types of evidence, evidence about different kinds of thing (monetary and
non-monetary, qualitative and quantitative), and for articulating concepts that
are not themselves evidential (such as equity).
It is not merely that processes can have characteristics that appeal in
and of themselves -- characteristics like transparency, citizen engagement,
openness, deliberation and contestability -- it is that characteristics such as
these are to be valued for more than their intrinsic merits. They are, in
short, necessary for the proper accomplishment of the tasks of HTA and, in
particular, they are essential to the major task of merging equity
satisfactorily with efficiency.
Philosophy, political science and social policy all address equity and,
in the case of philosophy, have done so for many centuries. Administrative
science, the law and management science have all addressed processes. But
none of these disciplines has concerned itself deeply with HTA (with the
exception of the sub-discipline of bioethics) and, typically, none has made the
theory and practice of HTA their daily business. This accounts, I conjecture,
for two unfortunate phenomena. The first is that the question whether the
methods of HTA ought to be more intimately linked to the processes of
real-world decision making has gone unaddressed. The two are treated as
essentially unrelated activities. As a consequence, HTA or at least the
conventional practice within HTA of cost-utility analysis has been described
as a perversion of
science as well as of morality (Harris 2005). Powers and Faden (2000) call attention to its
moral flaws, an unfortunate judgment that hinges on the implausible
proposition that those who use HTA methods, and CUA in particular, are moral
morons wedded to the uncritical use of a single decision tool. The charge is a
triple one: that the tool is a poor one, that it is used uncritically, and that
it is the only one they use. The other unfortunate phenomenon is that,
despite these centuries of study, no one yet has come up with usable tools that
would assist decision makers and those
who advise them to integrate the two great criteria of efficiency and equity
and to devise effective (even cost-effective) processes for doing so.
It seems to me that the way forward is for
those of us who are, as it were, HTA insiders should grasp the challenges
ourselves, perhaps in collaboration with some of the aforesaid colleagues from
other disciplines (including the critics), but at any rate not in deferment to
them, and set in motion a new research program designed to get to the heart of
these matters. That is what I propose to try to boost in the rest of this
paper.
Process
Arguably the biggest threat to
our public health care system is not our ability to pay for the increasing cost
of care, but rather a loss of public confidence. (Chase et al. 2010). While
this loss of confidence parallels a general scepticism about the adequacy and
fairness of public decisions across the board, health care has evidently not
escaped it. For many (e.g. Mendelberg 2002, Petts 2004) the solution is citizen engagement and other
processes of more direct democracy. I have much sympathy with sentiments such
as these. However, that is not where I want to lay the emphasis here. I want,
instead (or, perhaps, as well) to suggest that better processes would be
useful not only for re-establishing confidence in general, but also for
offering ways in which better decisions are likely to result. A better process might be better in the sense
that it is more transparent and confidence-building on that account. Those
are the intrinsic merits of a good
process and are embodied in accountability for reasonableness (Daniels 2000,
Daniels and Sabine 2008). But it may also be a better process by virtue of the
fact that it embodies more complete evidence, or more deeply investigated
evidence, or by its better combining of many elements -- some evidential and
others not, or through enabling a more complete addressing of equity and of its
consideration alongside efficiency. By process I mean the steps that are
taken, and their organisation and management, from the earliest inception of an
HTA (what technology is to be assessed?) through its further scoping and
refinement; selection of comparator technologies, identification of primary and
secondary research; critical appraisal of the evidence; stakeholder comment,
consultation and further deliberation; through draft guidance, recommendations
or decisions; appeals; conclusions, recommendations and dissemination.
The processes that I
particularly have in mind are: the possibility of external comment in order
that interested parties may see what there is to comment upon; consultation,
through which external parties are invited both to engage with decision makers
and their advisers and to enter into discussion about whatever aspects of the
process may be under way at the time, which includes assumptions, comparators,
model building, literature review and matters to do with the intrinsic process
itself; and finally, the most complete form of engagement, deliberation, in
which relevant stakeholders actually participate in the decision making itself
-- though probably excluding the final determination or conclusion of the
process, for which responsibility necessarily lies with those appointed to
decide.
Issues that require resolution
would be determined at a high level, such as through the board of an
organisation, or at ministerial or even cabinet level. Examples of such issues
include: specifying the objective (health maximisation?), the available budget,
the threshold (lintel?) ICER, the discount rate(s) to be used, whether
sophisticated programming or simple CEA is to be used, whether Multi-criteria
Decision Analysis is an approved method, the choice of technologies to
evaluate, and the comparators and equity requirements. Occasionally some of
these might be determined at a lower level, which I take to be the level of
the decision making agency or advisory committee. These lower level issues
would generally include all of the following: testing the concept validity of
outcome measures, assessing the quality of the science on a particular subject
intervention and its comparators, interpreting and combining both qualitative
and quantitative evidence (systematic reviews, other reviews, meta-analyses),
linking, if possible, internal and external validity, weighing uncertainty,
identifying absent information and deciding what to do in its absence,
assessing feasibility and manageable time lines, trading off conflicting
desiderata and, finally, making recommendations or issuing guidance through
(preferably tried and tested) Knowledge Translation methods.
A good many technologies do not
easily fit into the customary methods of HTA. Consider public health: its
complex interventions, diversity of responsibility for the vectors of delivery
(communities, schools, hospitals, prisons,
), heterogeneity of outcomes (better
health, but also reductions in teenage pregnancies, reduced crime, reduced fear of crime,
), long time horizons
(especially when the interventions involve culture change or challenge
cherished beliefs) and programmatic character (prevention, screening). Or
consider the simplifying assumptions, such as constant returns to scale,
non-diminishing marginal value of QALY, or the simple
additivity of outcomes, that are so often merely taken for granted rather than
tested for their appropriateness. Also consider the character of evidence,
especially when one widens the notion of technology beyond pharmaceuticals:
the greater dependence on multivariate observational studies and econometrics,
the use of cheaper experimental methods than RCTs, and the kind of evidence
required on value questions such as the value to be placed on a unit of outcome
or the measurement of changes in equity. Then too consider what might be best
regarded as a potential by-product of HTA: the possibilities it affords for
raising the public understanding of risk and uncertainty, the reasons why one
thing rather than another has been chosen, and the enhancement of the general
credibility of guidance.
The process has three
important aspects. One is to ensure that divergent views are properly
represented to minimize the chances that any one particular interest group
should unfairly capture the process. Another is to enable the wisdom and
experience of other decision makers to be brought to the table. Their
judgments, especially about value-laden and possibly controversial issues such
as quality of science or the meaning of equity, may be wiser than those of
the official participants. A third is that the process itself is a means by
which evidence is generated or at least brought before decision makers. Such
evidence might relate to matters of feasibility and manageability, where
the experience of practical managers amongst the decision makers may be a
useful input; to matters of external validity, where specific knowledge on the
environments into which an intervention might be introduced may be essential;
or to the appraisal of outcomes, where the fit of the outcome measures used in
research studies with the experience of actual patients and their carers can be
tested and possible biases identified and adjustments made on account of them.
(Culyer 2009, Dobrow et al. 2009)
I have just listed some issues and asserted some better ways of addressing them.
My selection is not evidence-based, save in a somewhat experiential and
necessarily partial way. Nor is it founded on any well-developed theory of
good decision making. It is therefore ad hoc. Most of the literature on these
topics, such as it is, is assertive rather than analytical, ideological rather
than scientific, strong on advocacy but weak on evidence. It is also written by
the practitioners of many different disciplines and appears in places that seem
very remote from any HTA concern.
Equity
Much the same applies, I fear,
to the treatment of equity. Of course, equity, in its major sense
of distributive justice and fairness has been a central concern of moral
philosophy since the days of classical Greece. Its modern students are
well-practised in the business of typology (utilitarian several varieties,
deontological again several varieties, theological, consequentialist, etc.
etc.) but they have, with a few fine exceptions. (such
as Daniels (2000) and Daniels and Sabin (2008) on decision processes, been
quite extraordinarily bad at providing tools for the use of practical decision
makers such as the practitioners and users of HTA
Even the most elementary
tools, such as a typology of characteristic equity issues to form an agenda
for discussion at various stages of an HTA process, would be an advance on what
we currently have. Such a typology might focus deliberation on such matters as
the domains of equity. For
example, there are equity issues regarding the use and distribution of health
care inputs, the processes that determine who gets what, the evaluation of
outcomes, and on the priority that ought to be attached to different diseases,
or to prevention versus cure. Decision makers need to reflect on the
appropriateness of the criteria used in respect of any of these, their
inclusiveness, the relative weight to attach to each, and so on. Some red flags
are provided in some jurisdictions by statute, as when there is a legal
obligation to guard against discrimination by age, gender, disability,
other demographics, workplace, education, institutionalized discrimination.
However, not all jurisdictions cover all possible issues and matters of
equitable concern may lie hidden in the depths of an HTA. There are also a
number of top level issues, such as whether there may be some principles on
which all would agree as minimal requirements for equity, whether it is
possible to enunciate some axiomatic statements that define what an increase
in equity might mean and how it might be recognised empirically, and there is
always a need to establish the applicability of any such principles in the
context in question.
Some of the hidden equity
biases that are likely always to need surfacing include embedded inequity through which possible unfairness is
built in to concepts (e.g. omitted dimensions of outcome measure that
discriminate against those for whom such outcomes are important), or framing effects in experimental
approaches that bring in social class bias, or unfairness that is inherent in
the intervention (e.g. a threat to autonomy through the removal of choice, as
with some public health measures). There are also institutional biases,
inequities resulting from practices in jurisdictional scope (e.g. health
consequences not taken into account by some faith-based provider institutions,
school boards or workplace managements) and the degree of concern many
jurisdictions have with the distribution of consequences (health or
not-health). There is also implicit stereotyping the use, often in all innocence, of
definitions and concepts that exclude individuals or aspects of health-related
welfare that have differential impact on individuals, and that make untested
assumptions about what does and does not matter to the people for whom the
intervention exists. Particular contexts (e.g. geography) may disadvantage some relative to
others. Minimally, surely, one ought to test to see whether any of the
following could affect the balance of advantage across different groups: the
setting of care (e.g. home or institution), language, education or SES of
clients, religious beliefs, stigma, or multiple deprivations.
Decision makers ought to ask, for example, whether the processes in HTA
itself are biased by denying representation to people with a legitimate
interest. Whether the interests of absentee stakeholders are properly considered
for example, those anonymous individuals for whom
services will not be provided as a consequence of implementing the
recommendations. Participants in HTA need to be self-aware and self-critical
regarding their own procedures. Processes
in delivery of the care under evaluation can be prejudicial to
technologies for some types of client (e.g. those of low SES) and can favour
those adept at negotiating their way through processes, or impose differential
burdens on some clients (e.g. wage versus salary earners).
Then there are special claims such as claims of need (e.g. low
initial health status?), of deservingness (e.g. choosing life styles that are
hazardous to health?), of history (e.g. past endurance of ill-health, past
receipt of the intervention), of desperation (e.g. last chance), of unfair
innings (lived only a short life-span), of non-health consequences (other
welfare effects), of willingness to pay (e.g. top-up payments). Sometimes the
beneficiary is identified as a member of a group or even by name as is often
the case with spectacular acts of medical or other rescue. Ought cases of extreme need be given special favour (Hope 2004 ch 3, Cookson et al. 2008)? What weight ought to be given
to such claims either in general or in the context of a specific HTA? What
weights actually are given (e.g. Cropper 1994, Johannesson
and Johanson 1997, Johanson-Stenman
and Martinson 2008)? Cumulative effects
may escape proper attention, for example, cumulative past disadvantages
or effects that might be relevant in assessing benefit or cost or their
distribution across patients and other affected groups.
The point of these examples is
that in the process of discussion and deliberation about a technology decision,
all of these hidden problems need to be deliberately surfaced because
ignoring them (being unaware of their existence, or
aware but doing nothing about them) leads to a bad decision. My suggestions are merely illustrative and
are certainly not exhaustive. But who better to complete the list, maintain it
through casuistry and careful recording of the reasons for decisions, and
synthesize and consolidate it over time, than those involved in the process of
HTA? Through such casuistry may we not build up case-based precedents to help
decision-makers achieve consistency across interventions and over time,
perhaps, eventually create a systematic ethics of HTA?
Deliberation
The slaying of both my dragons
HTA requires, I conjecture, deliberation, with an emphasis on: process, from
scoping a topic through evidence generation and synthesis to delivering
guidance; consultation with legitimate stakeholders (usually also a source of
evidence); and facilitated discussion. These all weak points in the current
state of HTA, and they are all Cinderella research topics (but see Lomas et al.
2005, Culyer 2009, Dobrowe et al. 2009) with multidisciplinary concerns.
I believe the ultimate product
and measure of success would be the increase in confidence of participants,
stakeholders and the public. This would be achieved by their understanding of
the processes and knowledge that the best evidence was used, that the
appropriate experts, lay and professional, had contributed, that all relevant evidence had been searched
and considered, that all relevant
stakeholders had their say and been heard, that key concepts (e.g. outcomes)
had been tested for construct validity, that all relevant cost and benefits had been weighed and included in calculations, that fair
comparisons had been made (both between interventions and between individuals),
that all relevant conceptual and empirical biases had been eliminated, and that
the main risks had been assessed and undue risks not taken. I suppose, taken as
a group, such outcomes might constitute evidence of a good process.
To realize this ultimate
product, however, HTA would be wise to broaden its horizons, turning away from
what is largely just an algorithm to find ways to take seriously the myriad
value and ethical issues which currently still have the unfortunate appearance
of afterthoughts, tacked on to, but essentially excluded from, the core
decision logic, and to develop an empirical program to rival, mutatis mutandis,
that of CEA and CER. After all, non-monetary values, though less easily
measured perhaps than monetary ones, are still subject to empirical estimation
and the values that individuals actually cherish ought at the least to inform decision makers values. This is
not merely a matter of expanding the algorithm but also, as I have tried to
show, a matter of developing suitable processes that generate information
through the participation of stakeholders while also facilitating the
thoughtful assessment of what is known, combining it with revealed values, and
producing multiple solutions to problems that are not uniquely soluble, like
those on which there are deep divisions of principle in the community. To
participate both in such processes and in the accompanying research program
must surely be one of the more exciting prospects confronting todays HTAers.
References
Brock DW. Ethical issues in the use of cost
effectiveness analysis for the prioritization of health care resources, in
Tan-Torres Edejert T., Baltussen
R., Adam T., Hutubessy R., Acharya
A., Evans DB., and Murray CJL (eds.) Choices in Health: WHO Guide to
Cost-Effectiveness Analysis, 2003, 289-312.
Chase R,
Levinson W, Hébert PC. The need for public engagement in choosing health
priorities, Canadian Medical Association Journal, 2010, DOI:10.1503/cmaj.101517.
Cochrane AL.
Effectiveness and Efficiency: Random Reflections on Health Services, London:
Nuffield Provincial Hospitals Trust, 1972.
Cookson
R., McCabe C., Tsuchiya A. Public
healthcare resource allocation and the Rule of Rescue, Journal of Medical Ethics, 2008 34:
540-544.
Cropper, M.L., Aydede S.K., Portney, P.R. Preferences for life saving programs: How the
public discounts time and age, Journal of Risk and Uncertainty, 1994, 8:
243-265.
Culyer AJ. Deliberative Processes in
Decisions about Health Care Technologies: Combining Different Types of
Evidence, Values, Algorithms and People, London: Office of Health Economics,
2009.
Culyer
AJ. The Dictionary of Health Economics, Cheltenham: Edward Elgar, 2010.
Daniels N. Accountability for
reasonableness: establishing a fair process for priority setting is easier than agreeing
on principles, British Medical Journal, 2000, 321: 1300-1301.
Daniels N., Sabin
JE. Accountability for reasonableness: an
update, British Medical Journal, 2008, 337: a1850.
M. J. Dobrow, R. Chafe, H. E. D. Burchett, A J Culyer, L.
Lemieux-Charles Designing Deliberative Methods for Combining Heterogeneous
Evidence: A Systematic Review and Qualitative Scan. A Report to the Canadian
Health Services Research Foundation, Ottawa: Canadian Health Services Research
Foundation, 2009.
Drummond
MF, Sculpher MJ, Torrance GW,
O'Brien BJ, Stoddart GL. Methods for
the Economic Evaluation of
Health Care Programmes. 3rd
ed. New York: Oxford University Press; 2005.
Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in
Health and Medicine. 1st ed. New York: Oxford
University Press; 1996.
Habermas J. The Theory of Communicative Action, Boston:
Beacon Press, 1987.
Harris,
J. Its not NICE to discriminate, Journal of Medical Ethics, 2005, 31: 373-375.
Hope
T. Medical Ethics: A Very Short Introduction, Oxford: Oxford University Press,
2004.
Johannesson, M., Johansson, P-O. Is the valuation of a QALY gained
independent of age? Some empirical evidence, Journal of
Health Economics, 1997, 16: 589 599.
Johansson-Stenman,
O., Martinsson, P. 2008. Are some lives more valuable? An
ethical preferences approach, Journal
of Health Economics, 2008, 27: 739-752.
Johri M., Norheim OF. Can
cost-effectiveness analysis integrate equity concerns? A
systematic review of current approaches. Paper at the
12th Annual ISPOR Conference, Paris, 2009.
Kuhn TS. The Structure of Scientific Revolutions, 3rd
ed. Chicago: Chicago University Press; 1996.
Lavery JV., Tinadana PO., Scott TW., Harrington LC., Ramsey JM., Ytuarte-Nunez CY., James
AA. Towards a framework for community engagement in global health research,
Trends in Parasitology, 2010, 26: 279283.
Lomas J., Culyer AJ.,
McCutcheon C., McAuley L., Law S. Conceptualizing and Combining Evidence for
Health System Guidance. Ottawa: Canadian Health Services Research Foundation,
2005.
Mendelberg T. The
deliberative citizen. In: MX Delli Carpini, L Huddy, R Y Shapiro
(eds.) Political decision making, deliberation and participation, Research in Micropolitics Vol. 6. Elsevier: Amsterdam, 2002.
Petts J. Barriers to participation and
deliberation in risk decisions: evidence from waste management, Journal of Risk
Research, 2004. 2: 115-133.
Powers, M. and R. Faden.
Inequalities in health, inequalities in health care: four generations of
discussion about justice and cost-effectiveness analysis, Kennedy Institute of Ethics Journal, 2000, 10, 109-127.
Reuzel, R.P.B.,
G.J. van der Wilt, H.A.M.J. ten Have, and P.F de Vries
Robbe, Reducing normative bias in health technology
assessment: interactive evaluation and casuistry, Medicine, Health
Care and Philosophy, 1999, 2, 25563.
**********************************************************************
An equity checklist: a framework for health
technology assessments
Anthony J Culyer, DEcon1* and
Yvonne Bombard, PhD2
1. Department of Health Policy, Management and
Evaluation, University of Toronto, Canada; Centre for Health Economics and
Department of Economics & Related Studies, University of York, UK
2. Department of Health Policy, Management and
Evaluation, University of Toronto, Canada
Introduction
A
challenge was recently presented to Health Technology Assessment (HTA)
practitioners to address equity better in their analyses [1].
In this paper we attempt to meet that challenge, at least in part. HTA is
the systematic evaluation of the consequences of the use of a health
care intervention (henceforth technology). Its principal purpose is to inform decision-making. Ethical
considerations and non-economic social consequences were included in early
general formulations of HTA [2].
However, it is only recently that attempts have been made to develop frameworks
for considering methods of integrating ethics and a wider set of social
consequences into HTA [3-7].
A comprehensive attempt to give practical guidance is that of the National
Institute for Health and Clinical Excellence (NICE) in England and Wales [6].
One important ethical consideration is equity. Despite the significance of
equity ideas in the design of many health care systems, pragmatic tools for
integrating them into the efficiency categories of cost-effectiveness in HTA
remain under-developed [8].
We attempt here a first step towards a pragmatic solution by providing a
framework of equitable considerations of potential relevance in HTA decision
making, giving examples of the ways in which such considerations might arise,
and providing a summarized checklist which may itself be used as a decision
tool by HTA decision makers or which could be further abbreviated as a desk-top
aide-memoire. The framework is primarily intended for high-level decision
makers who specify the criteria to be used by HTA advisory committees. The
checklist if offered as a first approximation to a practical tool for use by
such advisory committees.
Equity has many meanings in
both academic and lay contexts [9-12].
The absence of an agreed theory of
equity arises out of the absence of a general or monist theory of morality.
There are moral theories that claim to be general, such as utilitarianism,
though utilitarianism in its classical form is not directly concerned with
equity. Non-utilitarian theories hold, variously, that the equitable
distribution of health care resources is that which is to the advantage of the
least advantaged person - so-called maximin theory.
Deontological theory posits that an equitable distribution arises out of the
duty each has to provide for others. Entitlement theory holds that an equitable
distribution is the outcome of an equitable economic and social system (for a
review of rival approaches see Veatch [13]). We do not attempt the Sisyphean tasks
of selecting from or reconciling rival philosophies but suggest instead that
equity issues concerning the use of health care resources in a decision-making
context are best considered explicitly as pluralist. Rather
than defining a priori what equity is, we draw on a multidisciplinary
literature and our own practical experience, to create an eclectic list of
equity issues, which, if left unaddressed by decision makers, could be deemed
by a reasonable person to be unfair or to lead to unfairness in the adoption,
diffusion or consequences of a health technology.
Two domains of equity are
especially relevant in HTA. One is fairness of the procedures used in the conduct of HTAs. The other is equity as a decision criterion, like efficiency, for
ranking health care interventions.
Equity in the first sense has, at least in part, been conceptualized as
accountability for reasonableness [10, 14-16]
and has been adopted by some agencies
(e.g. NICE 2008). Equity in the second sense is a statutory requirement
in several jurisdictions and is likely to be increasingly required: illegal
discrimination will need to be addressed in all jurisdictions, such as the UK,
where such legislation exists. However, such imperatives typically address only
a subset of the concerns for equity that can arise in HTA. Unfortunately, there
exists no substantive body of principled thinking that can serve as a sure, or
even moderately agreed, foundation for a more comprehensive treatment of equity
in HTA [11].
Equity
in the sense of fairness in the way health care is financed, produced and
distributed has been a founding principle of many health care systems
throughout the world, and has resulted in systems that broadly fund activity
according to ability to pay and distribute it according to need (especially in
middle and high income countries). It would therefore seem appropriate for HTA
equity criteria in such jurisdictions to be at least consistent with these broader
ideals of health care. Unfortunately
there are major differences between definitions of need, measures of it and
its application in HTA decisions [12]
and it is far from clear what a criterion of need would require over and above
the criteria of effectiveness and cost-effectiveness.
The
standard approach to equity within HTA seems to operate at two distinct levels.
The first is general, such as being aware of the difference between horizontal
and vertical equity (noting that only the former involves attempting to achieve
equity through the equality of something [9, 17])
or having an equal respect for everyone. Since not all inequalities are
inequitable, nor all equalities equitable, we agree with Whitehead (1991) in
making equity and inequity the focus of our attention rather than equality or
inequality [18].
The second is specific, such as the application of differential weights to
costs and benefits according to particular equity-related characteristics of
those likely to be affected by the decision [19-27]).
While there is merit in this outcome-based approach, in practice decision
makers have difficulty in identifying circumstances in which departures from
strict equality in the value of units of outcome could be justified, with the
possible exception of end-of-life benefits which NICE, for example, explicitly
treats as warranting special weights, but without specifying them in
quantitative terms, and which others, such as Ontarios Committee to Evaluate
Drugs (CED), favour - though only implicitly. Equity-focused
impact assessments are examples of procedures that have a focus specifically
on the distribution of outcomes (e.g. Kemm et al 2006
[29]).
There
is little guidance concerning what, justly, ought
to constitute either the characteristics in question or the size of the
weights. Some gather evidence regarding the publics preferences, stakeholders perspectives or experts
advice on either of these matters [26, 27, 30-36].
Empirical efforts to discover what the public thinks about appropriate ways
of trading-off benefit with cost also raise the fundamental ethical question of
the extent to which HTA ought to
embody such values, even when participants are well-informed. It is possible that preferences may be
unstable or that the values elicited change according to the amount of
information that is given, the technology considered, whether the health state
in question is merely anticipated or actually experienced. Even when all such
confounders have been taken into account it is possible for there to be
considerable variance around population means and the distribution of ethical
values need not have a single mode. Ethicists might raise the objection that
what is just or fair is not to be determined by populist vote, while others
might contend that the preferences of elected representatives of the community
in question should count rather than the preferences of those who elected them.
Other methods have sought generalizable trade-offs
between equity and efficiency [37, 38].
However, not all equity issues involve trade-offs with efficiency [40]
and none of these approaches addresses what ought
to be done nor attempts to address the many other dimensions of equity that
ought to be taken into account. The dimensions of equity typically considered
(at least by health economists) are quite restrictive, being mostly concerned
with distributive fairness and focused on health, the geography of health care,
and income. Further, irreconcilable differences in values are glossed over,
hidden stereotyping happens and reliance, save in the case of legislated
requirements, is almost entirely upon intuition.
We
propose the creation of a pluralist [41]
checklist, that might be expanded and developed in the light of experience,
consultation, deliberation and the transparency that ought to accompany it. In
any specific decision context, not all the items in the checklist will be
relevant and perhaps none will be but the intent is to minimize the risk of
overlooking considerations of equity that might be relevant by ensuring that
minds are open to matters that can easily be overlooked or, if not overlooked,
that may be difficult to articulate, appraise or measure.
A proposed initial checklist
We
propose a practical and adaptable initial framework (the equity checklist),
as the basis for the development of a more comprehensive typology. It is practical
because it is intended as a sequence of red flags to alert decision makers
and the designers of the systems within which they work to matters of equity
that might warrant integration into the usual efficiency analysis of HTAs. It
is adaptable because the checklist as it currently stands is intended only as
an initial step and what may be added is currently unknowable (at least, by
us).
The
checklist is an initial framework to inform discussion and decision at a
relatively high level, to set criteria, and ensure that lower tier decisions
and the reasons for them are incorporated into minutes and notes of the
meetings at which they are taken, thereby enabling a dynamic process of
comparison and consolidation as cases accumulate. In our approach, what is
equitable or inequitable is less a matter for a priori definition than for discovery and subsequent
categorization by those appointed by legitimate means to make such decisions.
We hope that the checklist will help the process of discovering whether a
consensus does exist and, where it does not, what the nature of the conflict
may be and how it might most appropriately be dealt with.
Although
the exercise is not intended to generate a consensus, establishing that there
is no consensus on some of these questions is as important as seeking one [45].
While it may be possible to develop a consensus over time in a jurisdiction, or
at least a consistency in the way equity matters are considered, it seems
unlikely that such a consensus would ever be achieved across jurisdictions,
where prevailing standards, cultures and political values could vary greatly.
The
object instead is to enable all potentially relevant factors to be clarified
and considered, along with any evidence pertaining to them, including any
evidence generated in the actual process of consultation and deliberation. The
process is intended to affect both the procedures of the HTA as well as the final
appraisal determination. It may also be used
by agencies to determine the scope of equitable issues to be considered by
advisory committees, with the consequence that some of the matters identified
in the list would not in practice be open for discussion.
We
propose that the equity checklist should: (a) be used as part of the process
through which advisory bodies are given their terms of reference, (b) form a
part of the scoping agenda prior to the selection of a candidate intervention
and its comparators for HTA, (c) accompany the usual efficiency-related
statistical and analytical, research and background briefing for decision
makers, including systematic and other reviews, incorporating any anticipated
equity issues in the scoping stage; and
(d) where appropriate (e.g. when equity issues of sufficient weight are
identified to warrant detailed consideration) help to structure the discussion
and composition of multi-disciplinary, multi-professional and lay advisory
groups during the assessment process.
We
anticipate that the checklist will be developed in a variety of ways. One is
through academic research and discussion, which will in turn inform the
methodological guidance of HTA agencies. Others, which we have previously
characterised as casuistry, are through the gradual building up of case studies
of actual decisions, their reasoning, and their eventual analysis, synthesis
and consolidation into statements of good practice at various levels of the
decision making process. This will normally require digging deeper than the
mere on-line consultation of the recommendations and decisions of advisory
committees. In this fashion, we expect
to see an accumulation of case-based precedents that will help decision-makers
achieve consistency across interventions, constantly remind them of factors
that might otherwise be overlooked, together with suggestions of how they could
be handled.
Elements of the Checklist
Equity versus equality
Decision
makers may need reminding that equity and inequity are not the same as equality
or inequality. When, however, inequalities are linked with postulated causes as
when, for example, a concentration curve links health or ill-health to income,
an inequality might be judged as also inequitable. Some inequalities are actually
equitable as when, for example, someone with an urgent need to treatment
receives it before another who is a less urgent case. In all cases, however, it
is worth asking equality (or inequality) of what? Common candidates include:
need; deservingness or responsibility; capacity to benefit or be harmed; degree
of incapacity or current health state; history of past health or ill-health; prognosis with and without the technology;
health outcome - quality of life; and dependents (e.g. care-giving responsibilities).
The ethical element derives from the postulated cause of the health inequality.
Empirical causes judged to be ethically relevant commonly include income and
wealth; social class; social deprivation; and life-style and behaviour. While
the solution to inequity is likely to require addressing the underlying causes,
an assessment of their mutability and the balance of cost and benefit in
changing them, the range of remedies in HTA is typically narrower, lying within
health care and typically within a rather small subset of health care
technologies.
The
language of equality and inequality is explicitly quantitative and it is always
worth seeking empirical and quantitative information about how equal or unequal the relevant factors, outcomes or causes are
and how equal or unequal it is felt they ought to be. Major unjust inequalities
may rightly be perceived as more important to remedy than minor ones, though
the relative costs or redress ought normally also to be taken into account. In
all cases a judgement should be made as to whether the evidence on equity
warrants any significant departure from the implications of the efficiency
analysis, such as recommending the use of an intervention when its incremental
cost-effectiveness ratio is above that normally deemed to be the maximum
allowable, or not recommending one that is below that threshold, on grounds of
its inequitable consequences.
Domains of equity
The
matters for discussion under this category of the checklist relate to the appropriate
focus on equity, for example, whether it should relate to health care inputs,
processes or outcomes; whether it is the direct or indirect (perhaps
unintended) consequences of the
use and diffusion of the health technology that matter; whether there
should be a disease focus, with patients being classified by, say, diagnostic
group, or in some other way (say, by socio-economic status (SES)). If the
identification of subgroups within a larger class of individuals could generate
inequities, these should be explored. It is at this stage that some groups who
might be affected by a technology can be (innocently but mistakenly)
overlooked, as might be the case in interventions for parents that have
significant side-effects on children. Such an omission would, of course, also
bias an efficiency analysis as well as raising potentially significant equity
issues [46].
For example, if we consider a screening technology that distinguishes between
cancer patients who would benefit from a particular treatment from those who
would not, then one domain of equity pertains to the consideration the
implications for both sub-groups: not only the sub-group that benefits but also
those who are disappointed.
Legal Obligations
Most
jurisdictions will specify statutory requirements to consider justice and
equity and there may be further administrative obligations placed on agencies
by higher tier organizations or their own governing bodies. Anti-discrimination
legislation may be quite specific in requiring specific factors to be taken
into account and may go so far as to specify how and the discretion that is
permitted the decision makers. Legal obligations may be absolute, in the sense
that any inequality of the sort in question is illegal, or relative in the
sense that discretion may be exercised regarding the extent to which a given
inequality violates a principle of equity. Common dimensions include
discrimination by age, religion, gender, disability, ethnicity, race,
socio-economic status, nationality, language and sexual orientation. Other
dimensions may have regulations we cover under other headings.
General principles
Despite
the difficulty in obtaining universal assent to specific ethical principles, it
is always worth establishing whether some (probably simple) principles would in
fact be agreed for all cases or in the context of the case under consideration.
Some may be of inherently broadly applicable and become embodied as standard in
the consideration of equity. Principles that might be worth discussing could
include:
(a)
The domain of equity shall be current and prospective health not past health.
(b)
Equity requires either the attainable equality of something or else its fair
inequality.
(c)
Fair inequalities in treatment exist when the inequality arises from a fair
claim for being treated differently, such as an accepted claim of higher need.
It
may also be possible to agree specific axioms relating to equity, such as the
following cockshies:
Weak
equity axiom 1: if person A
has a worse state of health than person B,
then in determining the equitable allocation of an intervention having a given
impact on a population including A
and B the equitable
solution ought to increase As
health more than Bs, or reduce
it less.
or
Weak
equity axiom 2: if person A
has a worse state of health than person B,
then in determining the equitable allocation of a budget for interventions on a
population including A and B the solution ought to include
only interventions that on average increase As health more than Bs,
or reduce it less.
Embedded inequity
By
embedded inequity we mean inequities arising from inherent characteristics of
the analysis or intervention. This might arise from the use of specific
concepts or tools. For example, it is generally recognised that the use of
EQ-5D might discriminate unfairly against clients with cognitive impairment or
with sensory deficits for whom it is not well-designed. Unfairness might also
arise in the detail of the measurement process . EQ-5D may omit significant dimensions and
thereby unfairly discriminate against patients for whom the omitted factors are
key outcomes, such as relief of fatigue for people living with rheumatoid
arthritis or anaemia. Time costs may not properly reflect opportunity costs for
different social/employment groups, as when salary earners do not lose income
when attending a clinic compared with the self-employed. Practical measurement
and experimental methods may contain inequitable framing biases, or measures of
inequality may over or underweight the extremes of a distribution of benefits
or harms [48]
or exclude relevant dimensions [49].
The
systematic exclusion of vulnerable groups from clinical trials/research can
lead to an absence of evidence on effectiveness in those groups, which in turn
can result in inequitable denial of access. A now classic case of this bias is
the exclusion of women from cardiovascular clinical trials despite the
prevalence rate of cardiac disease amongst them (see Kim et al. 2009 [50]).
Embedded
inequity might also arise from the inherent character of an intervention, such
as denial of choice that can arise in some interventions such as water fluoridation,
population-screening programs or (healthy) fixed school lunch menus, where the
affront to freedom may bear more heavily on some than on others, such as those
with religious dietary restrictions. The commonly made assumption that a
quality-adjusted life year is of equal social value to whomever it accrues is
an embedded assumption that may need modification if it is thought that the
value (weight) placed on a QALY gain for one who is currently very sick ought
to be higher than for one less sick [23].
Inequity may
arise when the valuation basis of health outcomes is variable as when, for
example, those who have actually experienced a condition (and its treatment)
value its avoidance less than those who anticipate but have not experienced it [51].
More generally, if the prevalence of unstable valuations of outcomes is related
to other characteristics, such as education or social class, then a suitable
precaution might be to discover the views of those most directly affected by
the intervention in question. There is a great deal of evidence of the
considerable variability of preferences and valuations, and their
susceptibility to framing and other effects, in the literature of cognitive
psychology and experimental economics (e.g. Kahnemann
and Tversky 2000 [52]).
Institutional bias
Institutional
biases are those that are also embedded but in organizations rather than
analytical methods or interventions. The equity issue here is whether the
jurisdictional scope of agency or of its parent organization causes any costs
or benefits that might be significant for equity to be omitted or distorted.
For example, if major outcomes include effects such as reductions in teenage
pregnancies or a reduction in the frequency of j-walking, these may not be a
part of a Ministry of Healths remit, belonging instead to a Ministry of Social
Work or the Ministry of Transport. Conversely, the jurisdictional scope of
partner agencies or ministries might cause significant costs or benefits for
health equity to be omitted or distorted (such as impacts on life expectation).
Other skews
may exist in the distribution of the costs and benefits of interventions across
stakeholders that create inequity, as when workplace interventions have costs
that fall mainly on owners and benefits that fall mainly on workers [53].
Institutional biases may cut across a myriad of domains, including the highest
institutional levels such as health ministries, within agencies conducting
technology appraisals, in provider institutions, in workplaces and other
locations of care or intervention.
Implicit stereotyping
Implicit
stereotyping occurs when assumptions are made about a condition and the
desirability of treating it so as to ascribe those living with that condition
as abnormal or undesirable [54].
For example, individuals who are deaf like to consider themselves as a group
distinguished not only by deafness but also by a language (Sign) and resist the
descriptor disabled on the grounds that deafness is, in effect, a
socially-constructed disability, and therefore need not be treated.
Implicit stereotyping is especially likely when the culture of the patient
differs from that of the analyst. A dramatic example of the way in which
disease can be socially constructed is pinta (dyschromic spirochaetosis). This
skin disease produces distinctive rose-coloured spots on the
skin, which some Indians in South America once believed to be a sign of being
healthy, and which was so prevalent among some tribes that the few
single men not suffering from it were
regarded as pathological to the point of being excluded from marriage [55]. To treat it
therefore according to concepts of disease which are external to that culture is
likely to imply that the value of treatment thus estimated would conflict with
a value based on local Indian concepts and values. The danger for HTA
in implicit stereotyping is that the externally perceived health gain relative
to that perceived by the patient can be substantially different, and subsequent
implementation becomes patronising or even stigmatizing.
Implicit
stereotyping may be particularly expected for congenital and other chronic
conditions. A check is actually to ask the target populations concerned through
consultation and deliberation whether the measure or conceptualization of the
health benefit or state is biased or whether there may some members of the
target group for whom this might be the case.
Contexts, behaviours and circumstances
This category includes aspects of the
context of technology use that could, at least in principle, disadvantage some
people relative to others (e.g. traveling from a remote home to a clinic or
hospital) and thereby render an intervention cost-effective for one group but
not for another (e.g. [31]). Any of the following circumstances could affect the balance of negative and
positive consequences: demographics (age, sex, ethnicity, socio-economic
status (SES)), location of delivery of care (e.g. home or institution), language,
religious beliefs, sexual orientation, or multiple deprivation.
Some effects occur in unanticipated ways.
For example, it was found in Rich et al. (1976) that the reliability of
self-administered dipslide measures of bacteriuria taken at home by girls without symptoms varied
significantly with the age and socio-economic status of the children performing
the tests compared with costlier supervised sampling of the same girls [57]. In such cases, the cost-effectiveness of an intervention that
is in all other respects the same will be higher for the younger and/or lower
SES children.
There is considerable evidence that
differential behavioural responses to public health
measures according to SES may actually contribute in an unintended way to
inequity, especially when utilization of an intervention is lower among more disadvantaged and hard-to-reach populations or by
ethnic minorities [8]. It can be all-pervading, for which the term staircase effect was
coined by Tugwell et al. [58]. Unintended inequality-widening interventions have been termed
intervention generated inequalities [59]. These are widespread phenomena and have been found to exist, for
example, in many preventive interventions [60, 61]. There is also, needless to say, abundant
evidence that many interventions also generate greater health equality [58].
More generally, equity concerns may arise
whenever a particular technology is cost-effective for some subgroups of clients
but not others [38] whether for behavioural or other
reasons, depending again on the social and economic characteristics of the
subgroups.
Processes in HTA
Anticipated
equity effects that require adaptation of the usual review processes of the
agency need to be considered and addressed as early as possible in the HTA,
including the scoping stage. Thus, all questions concerning rights of different
groups to be consulted, represented or to participate
in decision making processes should be considered not only in terms of the
expertise, knowledge and understanding that they may bring to the process but
also with regard to fairness. For example, if a manufacturer or a patient group
may be affected for good or ill by the HTA process, it is likely that fairness
would at least require their right to participate to be considered.
If
the outcome measure of choice may not be valid for some patients, perhaps
because some aspect of health benefit is not included among the dimensions of
the measure, then the procedure should
ensure that decision makers have access to patients and informal carers with
experience of the condition and its treatment to enable the construct validity
of the measure to be assessed and, if necessary, to enable appropriate
adjustments. This approach was employed recently by the Medical Advisory
Secretariat in Ontario during their scoping stage of an HTA, where they sought
patient input on the research questions to ensure that they captured relevant
patient outcomes in their evidentiary review [31].
Hidden opportunity costs
These are costs imposed on
those affected by the intervention and anonymous people who are affected
through consequential changes in the distribution of resources. The identity of
the individuals who lose may not be known. The weight to be attached to any
such opportunity cost might vary according to what is known about who are most
likely to lose compared with those directly affected by the intervention. One
group of stakeholders that is almost invariably omitted from the deliberative processes
is the ordinary or potential
consumer of health care that is, members of the public (as distinct from
representatives of specific patient advocacy organisations). By definition,
these are anonymous individuals whose stakeholder status arises from the fact
that their taxes or premiums fund health care budgets, and if some of these
budgets are spent on one intervention, those parts are not available for others
including interventions for these ordinary and potential consumers. While this
opportunity cost provides the underpinning argument for using a test
incremental cost-effectiveness ratio (ICER) and is a conventional part of the
efficiency element of an HTA, the possibility arises that there may also be
equity considerations. For example, when the beneficiaries of a proposed new
intervention are relatively privileged or underprivileged members of the
community (or few in number) compared with the ordinary consumer. Similarly,
the ordinariness of those who bear the opportunity costs of newly introduced
interventions ought to be tested. Empirical ways in which this might be done
are, however, very much at the research stage.
Processes in the delivery of care
Processes in
the delivery of care might have inequitable consequences even in the absence of
institutional bias of the type already outlined. For example, the way in which
care is delivered may be demeaning or unduly revealing, as when a patient
enters an HIV or STD clinic having a sign publicly indicating its purpose.
There may be processes at local delivery sites that deny opportunities for
patients to reveal equity-related factors. For example, it is commonly charged
that middle class clients of health care systems are more adept at managing
their way through administrative processes and hence of receiving effective
health care [62].
A flagrant breach of equity arises when health care providers select out
patients deemed to be less financially advantageous to the organisation by
virtue, for example, of the chronicity of the disease
or their insurance status.
Special claims
There is a
range of frequently heard specific equity claims that ought to be anticipated
and appraised both in the scoping of an HTA and at subsequent stages. A
position should be taken as to what categories of claims will be entertained. Commonly met claims include: claims of need,
such as low initial health status; claims of responsibility, which may be
positive if, say, the likely beneficiaries are deserving by virtue of their
roles as, for example, parents, or negative if, say,the
likely beneficiaries are deemed undeserving by virtue of behaviour such as
pursuing life styles hazardous to health; claims of history, such as past
endurance of ill-health or previous receipt of the intervention; claims of
desperation, as when the intervention in question represents a last chance
for a cure; claims of unfair innings, such as a short already-lived life-span [63];
claims related to non-health consequences (other effects on welfare) or on
multiple deprivations; claims of willingness to pay such as a willingness to
top-up to compensate the provider for providing care that is less
cost-effective than the third party payers threshold requires.
Special
claims and possible inequity may arise in connection with individuals who are
not themselves patients. While it is commonplace in efficiency studies to
recognize the importance of taking account of the impact of technologies on
informal carers, carers too may have circumstances or characteristics that
warrant special consideration on grounds of equity, especially if they have carried
very heavy physical and emotional burdens while caring [64].
It is important not to be misled by spurious special claims from interest
groups but it is equally important not to allow the strongest of special claims
to go unappraised or to overlook the interests of those
who are not organized or equipped to ensure that their claims are.
Cumulative effects
The
consideration of cumulative past disadvantages or advantages that might be
relevant in assessing benefit or cost or their distribution across affected
parties would enable a broad view to be taken and help to ensure that the
whole was not taken uncritically to be merely the sum of the individual
parts. The accumulation might be across many equity categories, or over time,
or both. The possibility ought to be considered that such accumulation
strengthens any case for redress.
These
categories are summarized in the following checklist, in which we have
included prompts to stimulate discussion and the assessment of the relevance
of the category in question.
Table 1 about here
Conclusions
We
have provided a framework for developing a checklist of equity considerations
to complement the standard efficiency calculus of HTA. It is intended be used
as part of the process through which advisory bodies are given their terms of
reference; the scoping of the agenda prior to the selection of candidate
interventions and their comparators for HTA; the accompanying background
briefing for decision makers, including systematic and other reviews; and as a
tool to help to structure the discussion and composition of professional and
lay advisory groups during the assessment process. Its effective development
and implementation depends upon the creation of an on-going research program
that identifies omissions and on HTA processes that provide, through
appropriately detailed minuting and note-taking,
accounts of decisions taken by decision making agencies that can be interpreted
as precedents and analyzed retrospectively to promote consistency and to
understand the reasons why apparently similar cases have been adjudicated
differently on different occasions. Periodic reviews and updating guidance for
decision makers are also recommended. In these ways, it may be hoped that
equity will be more systematically and fully considered and implemented in both
the procedures and decisions of HTA.
Acknowledgments
Our thanks for their comments but absolution from
any responsibility for the contents of this article go to: Maria Benkhalti, Kalipso Chalkidou, Karl Claxton, Richard Cookson, Raisa
Deber, Mark Dobrow, Susan Griffin, Jan Hatcher Roberts, Murray Krahn, Mike Rawlins, Mark Sculpher, Peter
Tugwell, Erin Ueffing and
Vivian Welch.
References
[1] Culyer AJ. Hic sunt dracones: The
future of HTA one economists perspective. Journal of Medical Decision
Making. In press.
[2] Office
of Technology Assessment. Development of medical technology: opportunities for
assessment. Washington DC: U.S. Government Printing Office 1976.
[3] Lehoux
P, Williams-Jones B. Mapping the integration of social and ethical issues in
health technology assessment. Int J Technol Assess Health Care. 2007
Winter;23(1):9-16.
[4] Hofmann
B. Toward a procedure for integrating moral issues in health technology
assessment. Int J Technol Assess Health Care. 2005 Summer;21(3):312-8.
[5] Saarni
SI, Hofmann B, Lampe K, Luhmann D, Mäkelä M, Velasco-Garrido M, et al. Ethical
analysis to improve decision-making on health technologies. Bull World Health
Organ. 2008 Aug;86(8):617-23.
[6] National
Institute for Health and Clinical Excellence. Social Value Judgements:
Principles for the development of NICE guidance; 2008.
[7] Johri
M, Norheim, O.F. Can cost-effectiveness analysis integrate equity concerns? A
systematic review of current approaches. 2010.
[8] Cookson
R, Drummond M, Weatherly H. Explicit incorporation of equity considerations
into economic evaluation of public health interventions. Health Econ Policy
Law. 2009 Apr;4(Pt 2):231-45.
[9] Culyer
AJ, Wagstaff A. QALYs (quality-adjusted life-years) versus HYEs (healthy years
equivalents). J Health Econ. 1993 Oct;12(3):311-23.
[10] Daniels
N. Just Health Care. Cambridge: Cambridge University Press 1985.
[11] Brock
DW. Ethical issues in the use of cost-effectiveness alanysis for the
prioritisation of health care resources. In: Anand S, Peter, F., Sen, A.,, ed. Public Health, Ethics, and Equity.
Oxford: Oxford University Press 2004:201-23.
[12] Culyer
AJ. Need: the idea won't do--but we still need it. Soc Sci Med. 1995
Mar;40(6):727-30.
[13] Veach
RM. Ethical dimensions of the distribution of health care. New York: Praeger
1982.
[14] Daniels
N. Accountability for reasonableness. BMJ. 2000 Nov 25;321(7272):1300-1.
[15] Daniels
N, Sabin J. The ethics of accountability in managed care reform. Health Aff
(Millwood). 1998 Sep-Oct;17(5):50-64.
[16] Daniels
N, Sabin JE. Accountability for reasonableness: an update. BMJ. 2008;337:a1850.
[17] Culyer
A. Need - an instrumental view. In: Ashcroft R, Dawson, A, Draper, H.,
McMillan, J., ed. Principles of Health
Care Ethics. Chichester: Wiley 2007:231-8.
[18] Whitehead
M. The concepts and principles of equity and health. Copenhagen: WHO; 1991.
[19] Bleichrodt
H, Quiggin, J., . Characterizing QALYs under a general rank-dependent utility
model. Journal of Risk and Uncertainty. 1997;15:151-65.
[20] Bleichrodt
H, Diecidue E, Quiggin J. Equity weights in the allocation of health care: the
rank-dependent QALY model. J Health Econ. 2004 Jan;23(1):157-71.
[21] Dolan
P. The measurement of individual utility and social welfare. J Health Econ.
1998 Jan;17(1):39-52.
[22] Dolan
P. Desperately seeking numbers: the not-so-holy grail of the Super QALY. 20th
Nordic HESG Reykavic 1999.
[23] Dolan
P, Shaw R, Tsuchiya A, Williams A. QALY maximisation and people's preferences:
a methodological review of the literature. Health Econ. 2005 Feb;14(2):197-208.
[24] Dolan
P, Tsuchiya, A., . The elicitation of distributional judgements in the context
of economic evaluation. In: Jones A, ed. Companion
to Health Economics. Cheltenham: Edward Elgar 2006.
[25] Johannesson
M, Gerdtham U. A note on the estimation of the equity-efficiency trade-off for
QALYs. J Health Econ. 1996 Jun;15(3):359-68.
[26] Johannesson
M, Johansson PO. Is the valuation of a QALY gained independent of age? Some
empirical evidence. J Health Econ. 1997 Oct;16(5):589-99.
[27] Johansson-Stenman
O, Martinsson P. Are some lives more valuable? An ethical preferences approach.
J Health Econ. 2008 May;27(3):739-52.
[28] Department
of Health. A new value-based approach to the pricing of branded medicines: A consultation: United Kingdom Department of
Health; 2010.
[29] Kemm
J. Health impact assessment and health for all policies. In: Ståhl T, Wismar,
M., Ollila, E., Lahtinen, E., Leppo, K., , ed. Health in All Policies: Prospects and Potentials. Helsinki:
Ministry of Social Affairs and Health 2006:189-208.
[30] Giacomini
M, Hurley J, Gold I, Smith P, Abelson J. The policy analysis of 'values talk':
lessons from Canadian health reform. Health Policy. 2004 Jan;67(1):15-24.
[31] Bombard
Y. Public Engagement Pilot Study on Point- of-Care International Normalized
Ratio (INR) Monitoring Devices; 2009.
[32] Abelson
J, Giacomini M, Lehoux P, Gauvin FP. Bringing 'the public' into health
technology assessment and coverage policy decisions: from principles to
practice. Health Policy. 2007 Jun;82(1):37-50.
[33] Bombard
Y, Abelson, J., Simeonov, D., Gauvin, F.P. Eliciting social values and ethics
in health technology assessment: A participatory approach Social Science and
Medicine. Submitted.
[34] Nord
E, Enge AU, Gundersen V. QALYs: is the value of treatment proportional to the
size of the health gain? Health Econ. 2010 May;19(5):596-607.
[35] Nord
E, Daniels N, Kamlet M. QALYs: some challenges. Value Health. 2009 Mar;12 Suppl
1:S10-5.
[36] Cropper
ML, Aydede, S.K., Portney, P.R.,. Preferences for life saving programs: How the
public discounts time and age. Journal of Risk and Uncertainty. 1994;8:243-65.
[37] Williams
AH, Cookson RA. Equity-efficiency trade-offs in health technology assessment.
Int J Technol Assess Health Care. 2006 Winter;22(1):1-9.
[38] Ubel
PA, Loewenstein G. Distributing scarce livers: the moral reasoning of the general
public. Soc Sci Med. 1996 Apr;42(7):1049-55.
[39] Barr
N. Economics of the welfare state. Oxford: Oxford University Press 2004.
[40] Culyer
AJ. The bogus conflict between efficiency and vertical equity. Health Econ.
2006 Nov;15(11):1155-8.
[41] Brody
B. Life and death decision making. New York: Oxford University Press 1988.
[42] Ueffing
E, Tugwell, P., Welch, V., Petticrew, M., Kristjansson, E., for the Cochrane
Health Equity Field. C1, C2 Equity Checklist for Systematic Review Authors.;
2009.
[43] Tugwell
P, Petticrew M, Kristjansson E, Welch V, Ueffing E, Waters E, et al. Assessing
equity in systematic reviews: realising the recommendations of the Commission
on Social Determinants of Health. BMJ. 2010;341:c4739.
[44] Department
of Health. Health Equity Audit: A Guide for the NHS: United Kingdom Department
of Health; 2003.
[45] Karpowitz
CF, Mansbridge J. Disagreement and Consensus: The Need for Dynamic Updating in
Public Deliberation. Journal of Public Deliberation. 2005;1(2).
[46] Perry
CD. Does treating maternal depression improve child health management? The case
of pediatric asthma. J Health Econ. 2008 Jan;27(1):157-73.
[47] Littlejohn
P, Rawlins, M. Social value judgments: implementing the Citizens Council
reports. Patients, the Public and Priorities in Healthcare. Oxford:
Radcliffe Publishing 2009:109-23.
[48] Allison
P. Measure of inequality. American Sociological Review. 1978;43(6):865-80.
[49] Atkinson
A, Bourguignon, F., . The comparison of multi-dimensioned distributions of
economic status. The Review of Economic Studies. 1982;49:182-201.
[50] Kim
ES, Menon V. Status of women in cardiovascular clinical trials. Arterioscler
Thromb Vasc Biol. 2009 Mar;29(3):279-83.
[51] Kahneman D, Tversky, A. Choices, values and frames.
American Psychologist. 1984;39(4):341-50.
[52] Kahneman
D, Tversky, A.,. Choices, values, and frames. New York: Cambridge University
Press 2000.
[53] Culyer
A, Tompa, E., . Economic Evaluation of Interventions for Occupational Health
and safety: Developing Good Practice. Oxford: Oxford University Press 2008.
[54] Reuzel
RP, van der Wilt GJ, ten Have HA, de Vries Robbe PF. Reducing normative bias in
health technology assessment: interactive evaluation and casuistry. Med Health
Care Philos. 1999;2(3):255-63.
[55] Ackerknecht
EH. The role of medical history in medical education. Bulletin of the History
of Medicine. 1947;21:135-45.
[56] Frankel
S. The Huli Response to Illness. Cambridge: Cambridge University Press 1986.
[57] Rich
G, Glass NJ, Selkon JB. Cost-effectiveness of two methods of screening for
asymptomatic bacteriuria. Br J Prev Soc Med. 1976 Mar;30(1):54-9.
[58] Tugwell
P, de Savigny D, Hawker G, Robinson V. Applying clinical epidemiological
methods to health equity: the equity effectiveness loop. BMJ. 2006 Feb
11;332(7537):358-61.
[59] White
M, Adams, J., Heywood, P. How and why do interventions that increase health
overall widen inequalities in populations? . In: Babones SJ, ed. Social Inequality and Public Health.
Bristol: The Policy Press 2009:65-82.
[60] Katz
SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite
universal coverage. Breast and cervical cancer screening in Ontario and the
United States. JAMA. 1994 Aug 17;272(7):530-4.
[61] Alexander
FE, Anderson TJ, Brown HK, Forrest AP, Hepburn W, Kirkpatrick AE, et al. 14
years of follow-up from the Edinburgh randomised trial of breast-cancer
screening. Lancet. 1999 Jun 5;353(9168):1903-8.
[62] Dixon
A, Le Grand, J., Henderson, J., Murray, R., Poteliakoff E. Is the NHS
equitable? A review of the evidence. London; 2003.
[63] Williams
A. Intergenerational equity: an exploration of the 'fair innings' argument.
Health Econ. 1997 Mar-Apr;6(2):117-32.
[64] Zivin
K, Christakis NA. The emotional toll of spousal morbidity and mortality. Am J
Geriatr Psychiatry. 2007 Sep;15(9):772-9.
************************************************************
PET: a Practical Equity Tool for health
technology assessments
Anthony J Culyer, DEcon1* and
Yvonne Bombard, PhD2
1. Department of Health Policy, Management and Evaluation,
University of Toronto, Canada; and Centre for Health Economics, University of
York, UK
2. Yale University, Department of Public Health;
Memorial Sloan Kettering Cancer Center, Center for Health Policy & Outcomes
* Correspondence: Anthony J Culyer
University of Toronto
Department of Health Policy, Management and Evaluation
155 College Street
Toronto, Ontario M5T 3M6
Phone: (416) 978-7340
fax:
(416) 978-7350
e-mail: tony.culyer@utoronto.ca
No financial support was
received for this article. AJ Culyer is supported by the Ontario Government as
Ontario Research Chair in Health Policy and System Design at the University of
Toronto and has a part-time chair in economics at the University of York in the
UK. Y Bombard is supported by a Canadian Institutes of Health Research (CIHR) Postdoctoral
Fellowship and previously by fellowships from the CIHR Strategic Training
Programs of Public Health Policy and Health Care, Technology and Place.
Sponsors' support does not imply endorsement of the conclusions, for which the
authors retain sole responsibility.
Running Head: A Practical Equity Tool
Word count:
932 (excluding abstract, references and table)
1,877 (excluding abstract and references)
Abstract
Equity
refers broadly to fairness and provides an ethical underpinning for many of the
top level resource allocation principles of health care system design, the same
is not true in health technology assess ment (HTA)
even though equity is increasingly being considered by both theorists and
practitioners in a health technology assessment policy context. We advance our
previously developed conceptual framework on incorporating equity
considerations into HTA by presenting a table-top decision aid, which we call
PET: a Practical Equity Tool for HTA decision makers. We expect/hope that this
decision aid will help those who make decisions about the technologies for
which the insurance system (public or private) will pay to embody equity more
satisfactorily in their deliberations.
Abstract
Word Count: 79 (Limit: 250 words)
Equity
broadly refers to fairness and provides the ethical underpinning for many of
the top level resource allocation principles of health care system design in
both the distribution of services across client populations and the financial
contributions required of clients. Similar systematic building blocks cannot,
however, be said yet to underpin equity in the practice of health technology
assessment (HTA), even though equity is increasingly being considered by
theorists and discussed, albeit with little guidance, amongst some public
sector agencies engaged in HTA. In two recent papers [1, 2] we developed a
framework intended to help decision makers and their advisers to consider the
implications for equity that the introduction (or withdrawal) of health care
interventions, both clinical and non-clinical, might have. The idea was that
systematic consideration of the various elements in the proposed framework
might enable decisions that were hitherto based solely on cost-effectiveness,
and using only budgetary and health or service outcome information, or even on
sophisticated variations of the reference case recommended by the Washington
Panel [3], to be better informed in the future by explicit and systematic
consideration of equity. In principle, the consequences of such explicit and
systematic consideration could cut both ways interventions judged not to be
cost-effective for a specific subgroup may nonetheless be recommended on
grounds of their equity consequences, while interventions judged to be
cost-effective might not be recommended on account of their adverse equity
affects. Such bold steps, however, require a more secure footing than any
currently recommended methods prescribe. To this effect, we present a table-top
decision aid that we call PET: a Practical Equity Tool for HTA decision makers.
The
detailed framework is described elsewhere [2]. Here, we advance the arguments of
the earlier two papers in the form of a short checklist suitable for
encapsulation (lamination) as a table-top decision aid for HTA decision makers.
The summary presented here should be seen as a prototype. It is likely that
there are some aspects of equity that we have overlooked and which would need
to be incorporated in specific contexts. It is also virtually certain that in
some contexts and jurisdictions one or more of the included categories will
either prove irrelevant or need substantial amplification. These inclusions,
exclusions and amplifications ought to be accompanied by adequate minutes and
other records that explain the grounds for such decisions. Such minuting may then become casuistical precedents for
subsequent decisions as a cases build up. We hope, nonetheless, that at a
broad level of generality, the decision aid in its current form includes most
aspects that are likely to arise.
The
most effective use of the PET decision aid will depend on the quality of the
prior training of the participating stakeholders. Untrained and unprepared
deliberators, skilled though some of them may be in other aspects of HTA, will
be less effective than those for whom PET will prompt a recollection of more
complete arguments and other applications of equity principles, and a like
recall of facilitated simulations in training sessions. The items in the tool
are therefore also prompts, which may help those who design training and
guidance material.
We
expect that PET will require least adaptation at the highest levels of
decision-making, for example at the level at which a Ministry is instructing an
agency as to the categories to be considered, or at which an agency is
instructing its advisory committees. At lower levels of decision-making, such
as agencies like the National Institute for Health and Clinical Effectiveness
(NICE) in England and Wales or the Ontario Health Technology Advisory Committee
(OHTAC), or when manufacturers are deciding whether to make a case for their
products based on equity, the tool might omit categories that were not deemed
appropriate and it might contain more elaborate expensions
of aspects deemed to be of particular ethical significance.
There
are several ways in which the tool could be used. Possibilities include: help
to manufacturers in anticipating some aspects of the equitable or inequitable
impacts of their products, enabling them to provide agencies with information
supplementary to their usual cost-effectiveness material; inclusion as part of
the process through which advisory bodies such as NICE and OHTAC are given
their terms of reference; the identification at an agencys scoping stage of a
technology appraisal those aspects of equity that might lend themselves to
empirical research (quantitative and qualitative) and that might be undertaken
prior to any formulary-type decision; and where appropriate (as when equity
issues of sufficient weight are identified to warrant detailed consideration)
to help structure the discussion and composition of multi-disciplinary, multi-professional
and lay advisory groups during the appraisal process.
The above examples illstrate
decision-making contexts where PET may be applied. However, how
evidence, or opinion, about equity ought to be set against, or weighed up
alongside, the effectiveness and cost-effectiveness evidence is a matter for
deliberation between the decision makers and those whom they consult. Again,
good records of such processes and their outcomes would help to generate a body
of cases and provide evidence about the nature of the trade-offs considered
and the conclusions reached about them. Thus, we would strongly recommend that
such records be created and publicized, though where they might be publicized
is a matter for local consideration. We also hope that PET may serve to create
agendas for discussions between decision makers and researchers especially
those with expertise in equity and those with expertise in HTA and
cost-effectiveness analysis in health care and perhaps initiate on-going
dialogues between decision makers, through which pragmatic experiments and
experiences as they attempt to take equity more seriously can be shared.
![Text Box: PET: A practical equity tool for HTA decision makers
Guiding Questions:
1 Are we concerned with fairness related to equality or to fair inequality?
[Equality (or inequality) of what? Need, deservingness, responsibility, capacity to benefit (or be harmed), degree of incapacity or current health state, history of past health or ill-health, prognosis with and without the intervention; health outcome -- quality of life; and dependents (care-giving responsibilities)? Do we need quantitative information on any aspect? If there is any inequality of treatment or outcome, for example, by giving some groups a priority status, is it an acceptable inequality? What is the case for it? Is there any evidence base?]
2 Have all possible and relevant aspects of equity been taken into account?
[Should the focus of equity relate to health care inputs or costs, to processes or to outcomes? Might there be unintended consequences of an intervention that raise equity issues? Should the focus be disease or should some other basis for differentiating individuals and subgroups be used? Have equity aspects of the likely ways in which the interventions will be delivered been addressed? Have the Boards (or equivalent) equity requirements been met? Is there any evidence base?]
3 Have legally required factors been addressed?
[Have the relevant local legal obligations concerning age, gender, disability, ethnicity, race, nationality, language, sexual orientation, etc. been considered? Are there any legislative requirements concerning institutionalized, implicit or indirect discrimination?]
4 Are there any general principles of equity that ought to be taken into account?
[Have a set of guiding principles or axioms been established concerning what constitutes equality (or fair inequalities)? If so are they applicable in the current context? Is it possible to derive specific ways of proceeding from the general guidance? Are there any precedents from earlier decisions that we could draw upon?]
5 Are there any inequities embedded in our methods of analysis?
[Are possible inequities built into our concepts (such as omitted dimensions of outcome or cost), have there been biasing framing effects in experimental data, is there possible unfairness inherent in the intervention (such as a threat to some individuals autonomy)? Are the standard weights attached to gains and losses affecting different people (usually but not necessarily, unity) suitable in the current context? Do the empirical measures of inequity (if any) weight distance from the average in an acceptable way? Are there any indirect consequences of the intervention that may raise equity concerns?]
6 Is there any possibility of institutional bias?
[Do any of the following cause particular costs or benefits to be omitted or distorted: our parent organization, the culture of the manufacturers of the interventions, the culture of specific patient advocacy groups, the culture of the HTA experts and their institutions, provider institutions likely to deliver the intervention, workplaces?]
side one
© Anthony J Culyer and Yvonne Bombard 2011](welcome_files/image007.gif)
![Text Box: 7 Is there any possibility of implicit unfair stereotyping?
[Are we using definitions and concepts that inherently exclude or prejudice anyone? Do any aspects of the effects of the intervention have differential impact on individuals, or make untested assumptions about what does and does not matter, or stigmatize? Have assumptions about what matters been tested by consulting those affected? Are there people who might be affected but whose interests have not been taken into account?]
8 Could the current context and circumstances lead to inequity?
[Do any of the following circumstances affect the distribution of negative and positive consequences: geography, demographics (age, sex, ethnicity, socio-economic status), location of delivery of care (such as home or institution), education, language, religion, sexual orientation, or multiple deprivation? Are measures developed for one culture being appropriately applied in another (such as methods used in a high-income country being applied in a low-income country, or western values being applied in an aboriginal or first nations context?]
9 Are our HTA processes fair?
[Has the scoping of the HTA caused a bias in the processes through which information about equity has been gathered or considered? Is our procedure devoid of implicitly biasing elements such as the exclusion of relevant consultation groups? Have the appropriate stakeholders been included in the HTA process (including patients and members of the public)? Is anyone likely to have felt excluded?]
10 Have hidden opportunity costs been neglected?
[Has due regard been given to the interests of the anonymous clients of the health care system who are not the direct beneficiaries of the technologies being considered but from whom resources will be diverted as a consequence of the implementation of the recommendation of this HTA? Do those most likely to be affected in this way have distinctive characteristics suggesting that differential weights ought to be attached to the impacts on them? Are there any empirical estimates of any such relevant effects?]
11 Are the processes of delivery of the technologies equitable?
[Are there processes in the delivery of care, apart from those embedded in institutions, that discriminate unfairly? Are any of the likely delivery processes prejudicial to, demeaning of or embarrassing for some clients relative to others? Is there a middle class bias favouring those with skills at dealing with receptionists, bureaucrats, professionals and other unfamiliar groups?]
12 Are there any special claims that should be addressed?
[Are there interests such as people with needs that are not being heard? Do children, people near death require special consideration? Are their claims ethically significant? Can any claims that might carry weight bear empirical testing for veracity and size?]
13 Do cumulative effects matter?
[Has a holistic perspective been taken of people, or merely separate individual aspects? Have historical disadvantages been considered, especially multiple ones? Are there any other respects in which the cumulative experience or the combination of experiences of those affected may be of equitable concern?]
Side two
© Anthony J Culyer and Yvonne Bombard 2011](welcome_files/image025.gif)
References
1. Culyer, A.J. (2012) Hic sunt dracones: the
future of Health Technology Assessment one economists perspective, Medical Decision Making, forthcoming
Jan/Feb 2012.
2. Culyer, A.J. and Bombard, Y. (2012) An equity framework for health technology assessments, Medical Decision Making, forthcoming
May/Jun 2012.
3.
Gold M.R., Siegel J.E., Russell L.B. and Weinstein
M.C., eds. (1966) Cost-Effectiveness in Health and Medicine. New York:
Oxford University Press.
The NICE Cost Effectiveness Threshold what it is and what
that means.
Christopher McCabe#, Karl Claxton* and Anthony J. Culyer*+
#Academic Unit of Health Economics,
Leeds Institute of Health Sciences, University
of Leeds
*Centre for Health Economics,
University of York, England
+ Department of Health Policy, Management and Evaluation, University of Toronto
Acknowledgements
This paper is based upon a discussion
paper originally produced for the review of the NICE Guide to the Methods of
Health Technology Appraisal under the auspices of the DSU. We wish to thank
Louise Longworth, Carole Longson,
David Barnett and members of the DSU for constructive comments on earlier versions
of this paper.
Abstract
NICE has
been using a cost effectiveness threshold range between £20,000 and £30,000 for
over 7 years. What the cost effectiveness threshold represents and what the
appropriate level is for NICE to use, and what the other factors are that NICE
should consider, have all been the subject of much discussion. In this paper we
briefly review these questions, provide a critical assessment of NICEs
utilisation of the ICER threshold to inform its guidance and suggest ways in
which NICEs utilisation of the ICER threshold could be developed to promote
the efficient use of health service resources.
Section
1: Background
The
National Institute for Health and Clinical Excellence (NICE) is charged with
considering both the effectiveness and cost effectiveness of treatments and
then with making recommendations as to their provision within the National
Health Service (NHS). Cost Effectiveness Analysis (CEA) assesses two or more
alternative courses of action in terms of their costs and benefits. The
comparison is summarised using the expected Incremental Cost Effectiveness
Ratio (ICER). This is a measure of the additional cost per additional unit of
health gain produced by one intervention compared to another. NICEs preferred
form of cost effectiveness analysis uses the Quality Adjusted Life Year (QALY)
to describe the outcome of each intervention. By extension, the preferred form
of ICER is the Cost per QALY gained. Within the NICE appraisal process, the
ICER for each technology is compared to a threshold value; generally accepted
as having an upper limit of £30,000; to establish whether the technology
represents an efficient use of limited NHS resources.
The
objective of this paper is to review the current state of knowledge regarding
the cost effectiveness threshold, the principles of its use in health care
resource allocation decisions and any arguments for and against changing the
threshold from the current range of £20,000 to £30,000.
Section 2
summarises the current statements in the methods guide regarding the value and
of use of the cost effectiveness threshold. Section 3 reviews the relevant
literature on the use of the cost effectiveness threshold in resource
allocation decision making. Section 4
draws key implications of using an ICER threshold to promote population health
gain from the NHS budget. Section 5
considers the issue of whether the NICE threshold should change; and Section 6
attempts to summarise the key observations of the paper.
Section 2: What the current methods guide says
The current
methods guide refers several times to the cost effectiveness threshold. In chapter 6, (p33), it states:
The Appraisal Committee does not use a fixed ICER threshold
above which a technology would automatically be defined as not cost effective
or below which it would. Given the fixed budget of the NHS, the appropriate
threshold is that of the opportunity cost of programmes displaced by new, more
costly technologies. However, estimating this threshold would require complete
information about the costs and QALYs from all competing healthcare programmes
and the Committee does not have this information. Furthermore, the threshold
will change over time as the budget for healthcare changes. Although the use of
a threshold is inappropriate, comparisons of the most plausible ICER of a
particular technology compared with other programmes that are currently funded
are possible and are a legitimate reference for the Committee.Error! Bookmark not defined.
This statement acknowledges the importance of the
considering the opportunity cost of implementing new treatments given a fixed
threshold whilst conversely suggesting that, since the data required to
estimate the threshold quantitatively are not available, it is inappropriate to
use a threshold. Our interpretation of
this apparently contradictory statement is that it is use of a particular threshold that is to be
avoided, hence NICEs emphasis on a range.
The Guide then goes on to consider a range of
possible other factors to take into account, in cases of technologies with
ICERs at the lower and upper boundary of the range:
Below a most plausible ICER of £20,000/QALY,
judgements about the acceptability of a technology as an effective use of NHS
resources are based primarily on the cost-effectiveness estimate. Above a most
plausible ICER of £20,000/QALY, judgements about the acceptability of the
technology as an effective use of NHS resources are more likely to make more
explicit reference to factors including:
- the
degree of uncertainty surrounding the calculation of ICERs
- the
innovative nature of the technology
- the
particular features of the condition and population receiving the
technology
- where appropriate, the wider societal costs and
benefits. (p33)
This
approach echoes ideas advanced by Akehurst in 2002 and seems to
imply that NICEs effective threshold is actually £20,000 per QALY. When cost effectiveness ratios for a
treatment exceed this the Appraisal Committee considers (a) whether the
characteristics of the condition or population receiving the treatment would
lead them to value the health gain produced by the intervention more highly
than the estimate made in the analysis; (b) whether innovative characteristics
of the intervention are such as to require explicit consideration of the
Secretary of States instruction to give due weight to innovativeness, despite
the excess opportunity cost from a purely efficiency perspective; and (c) whether other benefits to society,
outside of those considered by the cost effectiveness analysis, are such that
it is socially desirable for the treatment to be made available.
The
proposed role of uncertainty in decision making is unclear. The text may mean
that when the ICER exceeds the lower bound of the threshold range, the
committee will seek greater levels of certainty to support a positive
recommendation. However, the text is
also consistent with Akehursts proposal that when
there is great uncertainty about an ICER in excess of the threshold value, it
is appropriate to the estimate as not significantly different from the
threshold value.
Use of
additional criteria such as these is not inconsistent with the operation of an
explicit, single threshold value, nor is it inconsistent with much of the
literature on social preferences over health care resource allocation. However, as we discuss below, there are
substantive issues concerning the ways in which such additional considerations
should be operationalised.
Section 3: Setting the cost effectiveness threshold
There
is significant argument about how the cost effectiveness threshold should be
determined. Three broad approaches have been proposed: (i)
it should be inferred from previous decisions; (ii) it should be set so as to
determine the optimal health care budget and (iii) it
should be set so as to exhaust an exogenously determined budget.
Inferring the threshold from previous decisions
Rawlins and Culyer, and Devlin and Parkin made two
attempts to infer NICEs cost effectiveness threshold from
reviews of previous decisions. The
former was an essentially qualitative analysis whilst the latter treated NICE
decisions as discrete choice experiments.
Rawlins
and Culyer identified an increasing likelihood of rejection as the ICER
increased beyond £15,000; with few interventions being approved with an ICER
> £30,000. Devlin and Parkin in
contrast estimated the threshold to be somewhat higher than the £20,000 -
£30,000 which NICE has publicly identified. (p450)
There
are several problems with basing the current threshold on previous
decisions. First, it is not necessarily
desirable for current decisions to use the same decision rule as for previous
ones; consistency of decision rule (the cost effectiveness threshold) can conflict with consistency of objective (maximising expected health gain). We discuss in more detail
why the threshold might change over time in Section 4. Second, this approach requires that that
previous decisions either took no account of any other considerations or that
any such consideration was judged not sufficient to have an impact on the
decision, otherwise the linking of particular ICERs to a particular threshold
value will have (largely unknowable) biases.
Settting the threshold to determine the optimal health care budget.
Some
have suggested that that the appropriate process is to identify the marginal
value that society attaches to health.
NICE itself has promoted two research projects
to examine what value people in the United Kingdom attach to an
additional QALY. If the cost
effectiveness threshold were set by such an empirically revealed monetary value
the implication is that interventions having an ICER below that value should be
approved. The health care budget would
then be whatever sum was required to implement the purchases. Setting the
threshold would thus effectively determine the NHSs budget. The budget would
be demonstrably consistent with the value that society attached to health and
the state would be committed to increase the budget so long as the ICERs for
new interventions fell below the threshold.
Three
approaches have been suggested for quantifying the marginal value of health:
discovering the willingness to pay for health gain of a representative sample
of society; using the value of life/health employed in other areas of public
sector resource allocation;Error!
Bookmark not defined. and
setting it equal to Gross Domestic Product per capita.
If
there were a direct link between societys willingness to pay for health gain
and the budget of the health care system, setting the threshold with reference
to it would seem appropriate. However, in the UK, as in many other countries,
the budget of the health care system is determined in large part by parliament
and is done (doubtless imperfectly) by broad assessments of the marginal value
of extensions of a wide variety of public programmes
and of the value of purchasing power left in the pockets of consumers. The
budget allocated to health care by parliament therefore already contains an
implicit value of marginal health gain - relative to alternative uses of public
funds It is difficult to see how experimental methods for revealing the social
value of a QALY could capture these opportunity costs more effectively (or more
legitimately) than Parliament. To substitute the direct democracy of public
opinion for a parliamentary process plainly also raises constitutional issues
well beyond the scope of this paper.
The health
care system is not the only area of public policy concerned with promoting
health. For example, transport investment decisions typically take account of
the expected impact on injury and death rates when appraising road building
schemes. It is therefore intuitively
appealing that the value of health ought to be consistent across public sector
activities. Loomes has suggested that
the ICER threshold should be set at a level consistent with the value attached
to a life in other parts of the public sector.
Whilst health and life are the primary (although not sole) objectives of
the National Health Service, they are not the primary objectives of other public
sector activities. The budgets allocated to these different activities by
parliament imply a relative valuation of these objectives as well as the impact
on health and length of life. It would be a major task to isolate the health
component in these other activities. Currently, only transport uses an
explicit value and, as one of us has previously observed, NICE simply does not have (and nor is it mandated
to acquire) the kind of information about outputs in non-health sectors that it
would need to form necessary judgements about the
marginal costs and benefits of health spending versus spending in other areas
of public services. (p11) Thus, although it may be intuitively appealing, it
is not feasible for the threshold to be set (by NICE)
by reference to other public sector activities.
Williams
suggested that a common sense value for the threshold would be per capita
Gross Domestic Product. At the time of
lecture this was somewhat lower than the bottom of the threshold range used by
NICE. The appeal of this proposal is
that if every member of society were to be given a fair share of nations
wealth, they would receive the per capita GDP. The maximum they could therefore
spend on health gain in any one year would be the per Capita GDP. Three significant
problems present themselves. First the approach implies that the society might
be willing to devote all its wealth to health care, which is manifestly not the
case. Second the same thought experiment will yield the same maximum for any good or service in GDP and so
provides no basis whatever for choosing between any of them. Third, the average cost effectiveness of health care can be at or below per
capita GDP with the cost effectiveness of marginal
programmes being markedly higher thanks to diminishing
marginal returns. NICE has to establish
whether a new intervention is more cost effective than the marginal
interventions that would have to be displaced in order to pay for it from a
constant budget. Use of an arbitrary
average risks rejecting interventions that were more cost effective than ones
already provided.
Setting
the threshold to exhaust a budget optimally
From
the beginning, NICEs use of cost
effectiveness analysis has been perceived as a means of promoting the efficient
use of available NHS resources. The cost effectiveness threshold ought thus to
be the cost per QALY of the least efficient funded treatment (i.e. the
intervention with the highest cost per QALY).
For a new intervention to add to health it must be more efficient per
unit of resource than the least efficient currently funded interventions and
ought to displace it in whole or part so that the marginal productivity of each
intervention in terms of health was everywhere equalized. Here too, however is
another evident informational challenge. If identifying the marginal
interventions for disinvestment is too difficult the threshold requires an
alternative justification. Here we need
to tread with care. On the one hand there is an issue of principle what the threshold ought to represent - a value judgement; and, on the other, an empirical question - the
value it should take in any specific context.
Figures
2a and b, reproduced from Culyer et al, illustrate the situation in which some
interventions not provided by the NHS are more efficient than some
interventions that are. If the function
of NICE is to substitute more
efficient interventions for less efficient ones, it can do this through
specifying a working cost effectiveness threshold, reflecting the Institutes
estimate of the ICER of the least cost effective activity undertaken by the
NHS. This working estimate is drawn from (a) the incomplete evidence base on
the cost effectiveness of interventions that the NHS does provide; and (b)
stakeholders personal and professional knowledge of the likely value of funded
interventions for which formal evaluations are not available. Over time this working ICER can be adjusted
in a casuistical fashion reflecting developments in the published evidence base
and evidence on the efficiency of disinvestments made to fund the recommended
interventions, changes in the health care budget and in judgments about the
efficiency of health care production.
Although
the threshold-searcher model describes how resource allocation processes can utilise ICERs for health care resource allocation decisions
at the margin, the authors did not address the frequently cited criticisms of
Birch and Gafni, who have repeatedly argued that
decision makers cannot maximize health gain from limited resources by using
ICERs in isolation from information on budget impact. To do so, they say, is a recipe for
continued expansion of expenditure. Their argument is that the opportunity
cost of a positive decision is determined by the total budgetary impact, not
the incremental cost effectiveness ratio. It is possible for the total budget
for an existing health intervention to be less than that for the new
intervention even though the new intervention has a lower ICER. If the new
intervention is mandated on the basis of the ICER alone, then extra funds would
need to be found.
The cost effectiveness threshold and the
budget impact
The
threshold searcher model can be used to explore the relationship between budget
impact and the cost effectiveness threshold.
The threshold is the inverse of the marginal health gain per unit of
expenditure of the least efficient intervention in current use. In Figure 2,
the substitution of a more for a less efficient intervention causes the
marginal health gain of the least efficient intervention to rise. As a result,
the threshold for future decisions decreases. The next candidate intervention
will need to be even more efficient in order to justify its inclusion as a
funded intervention. This is the case even if the budget impact of the
substitution is neutral, i.e. when the budget impact of the new intervention is
identical to the budget impact of the displaced intervention. Thus, the cost
effectiveness threshold is, as a matter of logic, endogenous once one allows
for dynamic interactions even though, in an overall sense, it is constrained by
the budget determined by Parliament.
To
the extent that the total cost of the new intervention is greater than that of
the procedure it replaces, a positive recommendation requires more
disinvestment until the budgetary impact of successive substitutions is neutral
and the budget constraint holds. This means that the cost effectiveness
threshold for an intervention with a large budgetary impact should be lower
than that for an intervention with a small impact. In this way, allocation processes based on a
cost effectiveness threshold can fully capture the opportunity cost of both
positive and negative investment recommendations.
The
rate of change of productivity also matters. Thus, when productivity is rising
through the use of relatively efficient technologies, the substitution of
generics for branded products, and so on, the health production function is
displaced upwards. As the budget
increases, the cost effectiveness threshold should also increase, i.e. less
efficient interventions should be incorporated into the portfolio of treatments
provided by the NHS provided that the productivity of existing health care
activities grows at a slower rate than the budget. In times of rapid expansion of the NHS
budget, such as have been seen over the past seven years, the countervailing
effects of the implementation of new treatments and increases in the budget may
have made the adoption of a cost effectiveness range a (fortuitously)
appropriate approach. Conversely, when
budgetary growth is less than the net budget impact of investment and
disinvestment decisions, the cost effectiveness threshold should fall to
reflect the increased efficiency of the marginal intervention. These relative
rates of growth of the budget and productivity of health care also have
implications, which do not concern us here, for discounting.
Summary
The
budget of the National Health Service is set by Parliament. NICE is charged to appraise the clinical benefits
and costs of such health care interventions as may be notified by the secretary
of state or the National Assembly for Wales
.and to reach a judgement
as to whether, on balance, this intervention can be recommended as a cost
effective use of NHS and PSS
resources. It is clear that NICE is not mandated to determine the budget of the
NHS and, since setting a threshold independently of the budget is logically
equivalent to determining the budget, NICE
cannot be mandated to do that either. The appropriate approach to NICEs cost effectiveness threshold is therefore to
see it as an equilibrating variable that promotes the efficient (health maximising) use of a fixed budget.
Section 4: Implications of
setting the ICER threshold to exhaust a fixed budget optimally
The ICER Threshold and Innovation
Figure 3
shows the total health gain to the NHS population under three scenarios. Consider an intervention costing £20,000 per
patient. At this price the ICER is below the cost effectiveness threshold and
the net health benefit of the intervention is one QALY per person. At a price of £40,000, the ICER is exactly
equal to the threshold and at this point the net benefit from the new
intervention is zero: the loss of health from displaced technologies being the same
as the gain.
However, if
the new treatment is more effective than existing treatments, then setting
price at a level that produces an ICER equal to the cost effectiveness
threshold implies that the full value of the innovation (greater efficacy) is captured
by the manufacturer. As the
manufacturers are typically profit maximisers they
will seek to price as close to this point as possible. Strictly, what is happening is that the
cost-effectiveness information is information not previously available to
manufacturers about the maximum willingness to pay of the demanders and makes
the task of perfect price discrimination, or the use
of an all-or-nothing demand curve more readily achievable by producers.
While it is
appropriate for manufacturers to appropriate a share of the value of
innovations it would be unwise to create a system under which they extract it
all. The public sector subsidises
research and development in a number of ways, through publicly funded research,
tax incentives and research infrastructure investment. Therefore, even if
society were unconcerned about who benefits from innovation (NHS patients or
the pharmaceutical industry) it would not be efficient to allow full
appropriation of the value of innovation by the manufacturer. However, society
is most certainly concerned about this distribution and it is reasonable that
at least some of the benefits of innovation should accrue to NHS patients. In pharmaceuticals, as in other industries
where innovation is protected, society currently permits monopoly rents during
patent protection but does not allow full appropriation by, for example,
facilitating perfect price discrimination.
Such
concerns as this are somewhat tangential to those of the Institute. Of direct relevance for NICE, however, is the
use of innovation as an argument for recommending interventions having ICERs
above the threshold. When the ICER is
close to, or at the threshold value, the full value of the innovation is
already being paid to the manufacturer.
To recommend an intervention when the ICER is above the threshold is to
pay more for the innovation than it is worth (in terms of the populations
health). Promoting population health is
consistent only with recommending treatments with ICERs that are below the threshold.
It seems inappropriate for NICE to seek to honour its obligations to promote
innovation through such a subsidy and at possible cost to NHS patients. NICEs
contribution to innovation is more likely to be realised effectively through
clarity and consistency in the criteria that it uses to make its
recommendations. The ultimate benefit is to bring the desire of the NHS to use
interventions that are no more costly than they need be into the research plans
of manufacturers so that the market is not disrupted by unforeseen changes in
requirements and innovation is of the sort that maximises and properly rewards
industrys contribution to the nations health.
The ICER Threshold and Equity arguments
While
efficiency, in the sense of health maximisation, is a major concern of NICEs
Appraisal Committee, it is not the only one, nor, indeed, is it possible to
identify efficiency without making assumptions about the relative value of
additional QALYs to different people. Interpersonal comparisons are therefore
inherent in the process of establishing efficiency. An important further
consideration relates to the wider opportunity cost of Appraisal Committee
decisions. When the threshold is being used to allocate a fixed budget, there
is not just one category of patient interest (those patients who would receive
the new treatment or some alternative) but two: in addition there are the
patients who bear the opportunity cost of its provision, i.e. those whose
service availability is reduced by virtue of the expenditure on the new
treatment.
We have
already observed that NICE does not know, and probably cannot know, which
patients bear the opportunity cost of its appraisal guidance. If NICE
recommends an intervention on equity grounds, it necessarily has to make
assumptions about the characteristics of those patients who bear the
opportunity cost. Specifically, in
making a positive recommendation, it must assume that the health gain forgone
of those who bear the opportunity cost is valued less than that of those who
receive the benefit.
Procedural
justice would seem to require that the character of the claims of the anonymous
bearers of the opportunity cost be properly considered in NICE appraisals. In
particular, when claims are made by advocacy and other groups about the special
nature, need, etc. of the people they represent, NICE appraisal must do their
best to assess the extent to which these claims carry greater weight than the
claims that could be made by those bearing the opportunity cost. Given the
typical pattern of NHS expenditure, the typical bearer of the opportunity cost
is, for example, likely to be elderly and in the last year of life. It does not
therefore appear intuitively plausible to suppose that the weight to be
attached to beneficiaries health gains must necessarily be higher than that
attached to the anonymous losers. Plainly this is an area in which information
is poor and broad generalisations will for some while have to substitute for
more specific identification of the characteristics of typical displaced
health gain. The matter is ripe for research.
Monitoring and recommending disinvestment
The current
methods guide avoids defining an explicit threshold on the grounds that the
correct figure cannot be known. However, both the previously suggested
casuistry (building up of specific cases) and the threshold searching model
imply that it may be reasonable for NICE
to utilise explicit thresholds which might converge over time on a best estinate. A crucial part of this search process would be
the identification of activities for disinvestment or, when there is budgetary
growth, to identify other planned investments that ought to be abandoned in
order to fund NICE recommendations.
There has
been little research either on selecting or implementing disinvestments in the
NHS. NICE has commissioned research from Brunel and City Universities
which has yet to be reported. Should it
turn out that actual disinvestments have tended to be more cost effective than
the NICE recommended interventions, there would be prima facie evidence for
supposing either that the current threshold is too high or that NHS trusts and
commissioners were making poor decisions at their levels. Discovering which the
case was would plainly be an important piece of work. However, it will not be
easy to discover. Local commissioners
choices will be determined by several factors including their total budgets,
cost structures, the case mixes of the populations they serve and even the ease
of implementation. As these factors vary across PCTs, the threshold is also
likely to vary by PCT, so whether NICE appraisal guidance has a positive or
negative impact on the efficiency of local health care will also vary by PCT.
Martin and
colleagues examined the actual changes in programme budgets and health across
Primary Care Trusts (PCTs) and estimated the average budget elasticity of
health, that is, the proportionate changes in health resulting from marginal
changes to programme budgets. They
provide empirical estimates of the cost effectiveness threshold expressed as
life years gained. They report a range from £7,397 for respiratory problems to
£26,453 for diabetes. The threshold estimates for cancer and circulation problems
were £13, 931 and £8,426 respectively.
These figures need to be interpreted with some care as they take no
account of the many interventions that impact upon quality of life rather than
survival. This said, the results are consistent with a
central estimate across all programme budgets around the lower limit of the
current range.
The
variation in thresholds between programme budgets has implications for NICE. It
implies that the opportunity cost of a NICE recommendation also varies
depending upon where it falls, so it may be efficient or inefficient dependent
on local circumstance. The risk of NICE Guidance being inefficient will depend inter alia on (i)
the degree to which national resource allocation captures geographical
variation in health needs; (ii) the degree to which local resource allocation
processes reflect variations in health needs between patient groups; and (iii)
whether the technology appraisal programme is focussed on those areas with the
greatest potential for increasing the efficiency of NHS activity. Local commissioners will almost certainly
need guidance on how best to identify and then manage disinvestments and
postponement of planned investments following NICE recommendations. It seems obvious that the criteria they use
ought not to conflict with those used by NICE (though doubtless supplemented by
further criteria).
Culyer et
al. suggested that NICE should
actively make both disinvestment and investment recommendations. The Institute has started to explore this
possibility. External organisations have also started to recommend that the
NHS, via NICE or other routes,
should disinvest from activities not having a robust evidence base. Most recently the House of Commons Select
Committee recommended that NICE
should appraise potential candidates for disinvestment; commenting that it was
unacceptable that the Institute had ignored the Committees earlier
recommendation to this effect. Unfortunately, the catalogue of procedures for
which the evidence base is poor or absent is very long and, where there is
advantage to be had from disinvestment, it is unlikely to be the case that the
scale of disinvestment required entails the entire elimination of a procedure.
So the task of specifying disinvestment guidance is by no means an easy one.
The use of
a cost effectiveness threshold is, at its core, about matching investment and
disinvestment to increase the total health produce by the health service. To
date, NICE has focussed its efforts on investment. Knowing what in fact is disinvested from can
provide some insight into whether, on average, NICE Appraisal Guidance is
improving the efficiency of the NHS. In the future, a programme of
disinvestment guidance, to balance the investment guidance might give the
public and the NHS greater confidence that the net benefit of the NICE
Appraisal Programme was positive.
Section 5: The changing threshold ICER
The Chair of NICE recently observed that the
current threshold range has been utilised for seven years and noted that the
Methods Review Process would need to consider whether the range should change
or remain the same.
Empirical estimate of the threshold
The House of Commons Health Committee
thought that the choice of threshold was of serious concern. The grounds for
this concern were that it is not based on empirical research and is not
directly related to the NHS budget. It seems to be higher than the threshold
used by PCTs for treatments not assessed by NICE.
(p68)
The Institutes response to the Health
Committees comments identified 17 technology appraisals that had produced
costs savings and stressed that most of the recommendations from the clinical
guidelines programme if implemented would save the NHS money. It went on to highlight the range of
knowledge promotion activities it is pursuing to promote efficiency in clinical
practice and commissioning. Whilst these are important and valuable activities,
it would seem appropriate, given the mandatory nature of Guidance from the
Technology Appraisal Programme, that the value of the threshold gives the NHS
and the people it serves, confidence that the opportunity cost of the programme
is less than the value of the health gain it produces.
Budget impact and the threshold ICER
A disadvantage of using a moving/converging threshold,
or one that was subject to periodic adjustment, is that it would evidently
introduce an additional uncertainty and provide a less secure environment for
industrial innovation. Whether this
additional source of uncertainty would be significant, given all the other
major uncertainties facing industry, such as the high failure rates in phase 3
drug development, is unclear. Current
pricing arrangements allow companies to amortize the cost of these failures through
the price of future successes, so the system may even encourage unnecessarily
high risk investments. Changes in the
threshold could be used to signal to the pharmaceutical industry and others,
the changes in the efficiency in the NHS that the Institute was established to
promote, and allow the industry to incorporate these changes into its
investment appraisal processes. This in turn would reduce the risk of
treatments coming to market which did not deliver sufficient additional health
gain to justify the price consistent with an acceptable return on investment.
What would also help would be the wide promulgation of the principles upon
which changes in the threshold would be made, thus enabling future changes to
be anticipated.
Should the threshold ICER change?
The
empirical evidence of Martin et al. indicated that even the lower end of the
current cost effectiveness range may be too high and likely to lead to less
efficient treatments being implemented at the cost of more efficient ones. The
Select Committee report observes that the current threshold is higher than the
ICER used by PCTs in their commissioning processes. Thus, there is a prima facie case for
considering reducing the threshold. However, it maybe premature to
substantially change the threshold on the basis of the current narrow range of
studies.
The
efficiency of NICE Guidance may be promoted without changing the threshold. The
current methods guide indicates that £20,000 is the threshold at which other
criteria than the ICER come into play. A
substantial proportion of the treatments approved by NICE have been in this
range. Modifying the utilisation of
these other factors in line with the arguments we have set out, would have
the effect of strengthening the lower bound of the current range as the
effective threshold and thus promote the efficiency of future NICE Guidance.
Section 6: Summary
The
incremental cost effectiveness threshold, as used by NICE, is a means for
promoting the optimum allocation of a fixed budget. It is not necessarily an
expression of societys willingness to pay for health. Using the threshold searcher model described
by Culyer et al to explore the implications of this, we conclude that:
(a) it is
feasible and probably desirable to operate an explicit single threshold rather
than the current range;
(b) the
threshold should be seen as a threshold at which other criteria are taken
into account beyond the ICER itself
(b) interventions
with a large budgetary impact may need to be subject to a lower threshold as
they are likely to displace more than the marginal activities;
(c) reimbursement
at the threshold transfers the full value of an innovation to the
manufacturer. Positive decisions above
the threshold on the grounds of innovation reduce population health;
(d) the value of the
threshold should be reconsidered regularly to ensure that it captures the
impact of changes in efficiency and budget
over time;
(e) the use of
equity weights to sustain a positive recommendation when the ICER is above the
threshold requires knowledge of the equity characteristics of those patients
who bear the opportunity cost. Given the barriers to obtaining this knowledge,
and knowledge about the characteristics of typical beneficiaries of NHS care,
caution is warranted before accepting claims from special pleaders.
(f) uncertainty in the evidence base should not be used to
justify a positive recommendation when the ICER is above the threshold;
(f) the
development of a programme of disinvestment guidance would enable the Institute
and the NHS to be more confident that the net health benefit of the Technology
Appraisal Programme was positive.
Figure 1: Relationship between cost effectiveness and
probability of rejection (Rawlins and Culyer)
Figure 2: NICE as a Threshold
Searcher
Searching for a threshold,
not setting one:
the
role of the National Institute for Health
and
Clinical Excellence
Anthony Culyer, Christopher McCabe, Andrew Briggs, Karl Claxton, Martin Buxton,
Ron Akehurst, Mark Sculpher, John Brazier
Introduction
The quality-adjusted life-year (QALY) is the outcome measure
of choice in England and Wales for the National Institute for Health and
Clinical Excellence (NICE).1 There has been much speculation about whether NICE
has a threshold figure for the cost of an additional QALY above which a
technology will not be recommended for use in the National Health Service
(NHS), and there has been some suggestion that NICE is dissembling in its
denials that such a threshold exists.2 Retrospective analysis of appraisal
determinations in its first year of operation suggested that positive
recommendations were in general associated with a cost per QALY of £30,000 or
less; higher cost per QALY figures would receive approval only if there were
special factors accepted as relevant and not covered by the formal modelling.3
Attempts to infer what any such threshold might be, based on
published appraisal decisions, have identified a general concentration of
estimates in the region of £20,000£30,000 in one study2 and a suggestion that
the threshold might be considerably higher than £30,000 in
another.3 In April 2004, NICE
confirmed that interventions with a cost per QALY below £20,000 were likely to
be recommended, while the acceptability of therapies between £20,000 and
£30,000 per QALY is more likely to depend upon other factors, such as the
innovative
nature of the therapy.1 Prior to this, the only published
specific threshold came from the Department of Health4 in which a threshold of
£36,000 was set, specific to a risk sharing agreement with the pharmaceutical
industry over the provision of disease-modifying drugs for people living with
multiple sclerosis. There are good reasons why it is improper for NICE to apply
a specific threshold. NICEs proper function is as a threshold-searcher,
seeking to identify the optimal threshold that lies somewhere between the least
cost-effective technology currently provided and the
most cost-effective technology not yet available routinely in the NHS. It is
not constitutionally proper for NICE to determine the threshold.
NICEs function in relation to appraisals is to appraise the
clinical benefits and the costs of such health care interventions as may be
notified by the Secretary of State or the National Assembly for Wales and to
reach a judgement on whether on balance this intervention can be
recommended as a cost-effective
use of NHS and PSS resources.5
The logical implications of NICEs mandate can be made clear
in the following way. Consider a rank ordering of all the technologies
available to the NHS and the most efficient ways of spending NHS funding, as
shown in Figure 1. Those that have the largest possible impact on health per
pound spent are plotted on the left with each addition to health gain falling
as people with the best chances of being helped have already been
helped. The downward slope
continues until the point E is reached, at which the available NHS budget has
been used up. The height of the line at this point (Ea) shows the marginal
health gain (mhg) from additional expenditure, given
the current budget. Its inverse shows the marginal cost-effectiveness of NHS
expenditure, or the threshold incremental cost-effectiveness ratio. The total
health gain produced by this expenditure is the entire area under the curve. It
is the greatest gain in health achievable, given the range of technologies
available and the current NHS budget. It requires that this budget is
effectively spent by the NHS so that none of the technologies with an mhg less than Ea is used. If
the objective is indeed to maximize the impact of health services on health,
then we can approach the defining characteristic of this objective in either
one of two ways. We can either speak of a budget that is to be efficiently
spent, which entails using all the technologies embodied in the figure up to
0E, which implies the threshold mhg of Ea; or we can
speak of a threshold QALY gain per unit of expenditure Ea, which entails
using all technologies
whose mhg is higher than Ea, which will (just)
require a budget of 0E. The two are equivalent: we may either spend the budget
to maximize health (which implies the threshold), or purchase all technologies
up to the threshold (which implies the budget). Both produce the same outcome.
Determining the budget is Parliaments business. NICE is
neither mandated nor qualified to make judgments about the relative value of
public money spent on health care versus education, defence, environment, etc.
and, of course, private consumption. But, since determining the threshold is
logically equivalent to determining the budget (given the available
technologies embodied in the curve), NICE cannot be qualified to pronounce on
that either. Therefore, information about how much an individual or society
values improvements in health (i.e. their willingness to pay for a QALY) is not
at all relevant to the NICE remit. These values could only be used as the
appropriate threshold by NICE if it were also given responsibility to set the
NHS budget. NICE as a threshold-searcher The
information demands of optimizing NHS expenditure are manifestly huge. NICE has
incomplete and uncertain information on the mhg
function in Figure 1 and, therefore, does not know the value of the
threshold. The threshold is
neither taken by NICE (from government) nor made by NICE. NICE is neither a
threshold-taker nor a threshold-maker. NICE is, in effect, a
threshold-searcher, where the threshold is logically implied by the combination
of the technologies that are available and the budget, but is not readily
visible.
Figure 1 assumes the NHS is able to allocate its budget on
programmes in order of their health gain per pound spent. Figure 2 explores the
more realistic analytical problem for NICE when the current budget is not
allocated in this efficient manner. In Figure 2, the range of technologies in
0E embodies those in the NHS. Let us assume that all are positive and that the
least productive one has, as before, an mhg of Ea. However, we now assume that there are many
technologies that are not currently provided within the NHS. These technologies
are ranked in a separate
downward-sloping function to the
right of E labelled cf. A composite mhg curve is the
horizontal sum of the two lines, Hde, which combines
all available technologies: those in use as well as those that could be used
but are not, and again orders them by contribution to health gain. It is
immediately apparent that NICE confronts three potentially interesting mhgs, the size of none of which it can be sure of. Ea is
the actual mhg implied by current use in the NHS. It
is what the current threshold would appear to be if a comprehensive
assessment were to be made of the ways in which NHS resources are used. Ec is the health gain to be achieved from adopting the best
technology not currently in use. Eb is the threshold
above which technologies ought to be adopted and below which they ought not.
The incorporation of any technology not in current
use with an mhg above Eb would represent an
increase in health gain as long as it displaces a technology with a lower mgh (in the range E0E). The optimal solution is plainly to
cease using all those technologies in the range E0E on Ha and substitute for
them all those in the range
EE00 (¼E0E) on cf.
The search strategy for NICE is to work within the zone of
substitution, defined by E0E00, identifying technologies in current use that
are the least productive uses of current NHS resources, and identifying better
value technologies that are not currently provided.
NICEs search strategies It is not feasible for NICE to
examine the cost-effectiveness of all interventions to reveal the location of Hde. Instead, NICE adopts a number of strategies consistent
with the behaviour to be expected of a threshold-searcher. In collaboration
with the Department
of Health, it engages
in horizon scanning to explore technologies that probably lie in the zone of
substitution. NICE also relies upon a broad consultative process with all
stakeholders, including the general public, to identify technologies for both
investment and disinvestment. The proposals obtained through the consultation
process inform which therapies to put forward for review.6 Within
the review process, the
appraisal committees
judgments on the cost effectiveness of a new technology must include judgments
on the implications for health care programmes for other patient groups, how
the cost effectiveness of the technology being appraised relates to other
interventions/technologies currently being applied in the NHS.
If this system were to work well, we would expect to see a
mixture of investment and disinvestment opportunities being reviewed by NICE.
However, in practice almost all NICE appraisals have only considered
opportunities for investment,7 leaving consideration
of disinvestment opportunities to local purchasers. While some of the latter
have established formal processes for considering local disinvestment and
investment decisions,8,9 there is substantial variation in
both the quality and the degree of transparency in such processes.10 In view of
this, a common evaluative framework producing information on the
cost-effectiveness of a larger range of technologies might help to make a
bridge between local purchasing and NICE. For example, NICE could work with
local purchasers to identify programmes and technologies for which there exists
a prima facie case for disinvestment. It could then appraise
these over time together with emerging technologies, in the expectation of
providing a more balanced set of investment and disinvestment opportunities.
Conclusions
It is not NICEs constitutional role to determine the value
of an additional QALY since the setting of the NHS budget is properly a matter
for parliament. NICE, nonetheless, needs a criterion on which to judge the
cost-effectiveness of technologies that pass through its appraisal process and
it is the search for the threshold implied by the prevailing NHS budget that is
the appropriate task for NICE. This will require NICE to grasp the
disinvestment nettle and include within its current appraisal process
technologies that should no longer be provided as well as candidate
technologies to replace them.
Acknowledgements
We acknowledge the valuable comments on early drafts of this
paper from Nancy Devlin, Andrew Dillon, Alistair Fischer and Adrian Towse.
References
1 National Institute
for Health and Clinical Excellence. Guide to the Methods of Technology Appraisal. London: NICE, 2003
2 Towse A, Pritchard
C.
Does NICE have a threshold? An external view In: Towse A, Pritchard C, Devlin N, eds. Cost-Effectiveness Thresholds: Economic and
Ethical Issues. London:
Office of Health Economics, 2002;2537
3 Devlin N, Parkin D. Does NICE have a
cost-effectiveness threshold and what other factors influence its decisions? A binary choice analysis. Health Econ 2004;13:43752
4 Health Service
Circular 2002/004. Cost effective provision of disease
modifying therapies for people with multiple sclerosis. Available at
http://www.dh.gov.uk/assetRoot/04/01/22/14/04012214.pdf (accessed 21 November
2005)
5 NICE. Framework
Document. Available at
http://www.nice.org.uk/pdf/appendixB_framework.pdf (accessed 21 November 2005)
6 NICE. How topics are
suggested and selected for NICE 10 steps.
http://www.nice.org.uk/pdf/topicsuggestionppslideshow.ppt (accessed 30 November
2005)
7 NICE. Published
Appraisals. http://www.nice.org.uk/page.aspx?o=appraisals.completed
(accessed 30 November 2005)
8 Evidence Based Commissioning
Collaboration. http://www.trentrdsu.org.uk/resources_evidence_about.html
(accessed 30 November 2005)
9 West Midlands
Health Technology Assessment Collaboration. http://www.pcpoh.bham.ac.uk/publichealth/wmhtac/
(accessed 30 November 2005)
10 Hoffmann C, Stoykova BA, Nixon
J, Glanville JM, Misso K, Drummond MF. Do health-care
decision makers find economic evaluations useful? The findings of focus group
research in UK
health authorities. Value Health 2002; 5:718
Equity in economic evaluations of workplace health and safety
Anthony J. Culyer and Emile Tompa
A basic tenet of economics is that
resources are scarce, so it is in the interest of individuals and societies to
put them to their best uses. This is the notion underlying allocative
efficiencyto get the most for the least. Economic evaluation is a tool to
assist with achieving it. Invariably, it requires placing values on both the
resources consumed and the consequences their use has produced in order to
compare inputs and outputs within and across alternatives. Also inherent in the
process is the need to compare and, where appropriate aggregate, costs and
consequences across individuals and groups.
Allocative efficiency is a central objective
in economic evaluation, but equity is equally important. Equity is commonly
considered to be of two main kinds: distributive equity/justice, which refers
to the fairness of the allocation of benefits and burdens, and procedural
equity/justice, which refers to the fairness and acceptability of decision
making processes (see Box
1 for definitions).
Box 1: Key efficiency and equity
constructs
Within the broad equity constructs
of distributive and procedural justice there are many rival notions. All have
it in common that they embody values, so none can be assessed solely on
scientific terms. They are also based upon an idea of distancing the
balancing of conflicting interests in a way that is detached from personally or
institutionally selfish interests. They are intended to inform behaviour or decisions that help answers
questions such as: how ought management choose between alternatives?, should
monetary costs and consequences accruing to workers be valued the same as
monetary costs and consequences to employers?, what is a fair distribution?,
what is the fairest way to prioritize occupational health and safety (OHS)
options (within a workplace, a region, or a jurisdiction)?. Equity concepts,
both distributive and procedural, involve more than one person; they are about
relationships and comparisons of people (both individuals and groups). In
short, they are about making interpersonal comparisons.
Equity (or its absence) is a
characteristic of a society. It is usually treated at the macro (country,
societal) or meso (system) level but in some cases is
it treated at the micro level, where, perhaps, no more than two people are
involved, as for example in physician-patient relationships. In the health
economics literature, textbooks such as McGuire et al. (1992), Mooney (1992), Dolan and Olsen (2002), Folland et al.
(2004), and Donaldson et al. (2005)
focus on macro and meso equity issues associated with
health care system design and evaluation. Few discuss the central topic of this
chapter: the microeconomics of economic evaluation using CEA, CUA and CBA
methods. We discuss macro and meso level equity, but
try also to provide some initial guidance on how best to address equity issues,
of whatever kind, in the context of economic evaluations of OHS interventions.
Since equity is a topic in several
disciplines, we recommend a few references as a starting point to scoping out a
vast literature. For a review of equity from a general philosophical
perspective see Plant (1991). For a review of equity from a general economics
perspective see Hausman and McPherson (2006), and for
a more specific health-oriented philosophical perspective see Daniels (1985).
Williams and Cookson (2000) provide a good review of the equity literature
focusing on the macro and meso health economic
perspective. Wagstaff and van Doorslaer (2000) also
provide a review of the health economics perspective but with a focus on
finance and delivery.
Equity and Equality
There
is an important characteristic that concepts of equity have in common-- they
all have to do with equality or inequality. Thus it becomes important to ask
the question: equality or inequality of what? Equity does not equate to
equality, however. Sometimes one deals with just inequalities and the
question is then what is the criterion for deciding which inequalities are
fair or unfair? Equity thus means treating likes alike and unalikes
appropriately differently. It requires that relevantly similar cases be treated
in similar ways, and relevantly different cases be treated in appropriately
different ways. This brings to the fore two important concepts: horizontal
equity and vertical equity. Horizontal equity
is the equal treatment of people who are equal in a relevant respect. Vertical
equity is the unequal treatment of people who are unequal in a relevant respect
(see Box 2
for details). It also requires us to be clear about what factors count as
relevant respects.
In
the context of OHS interventions and the associated costs incurred and consequences
produced, equal or unequal treatment for the purpose of fairness or equity
amounts to assigning priorities to costs and consequences accordingly. As has
been seen in previous chapters, many research studies arbitrarily restrict the
categories of cost or consequence considered, for example by ignoring costs or
consequences that fall on workers families, or by attributing an implicitly
high weight to positive productivity effects on the bottom line or by
minimizing the negative consequences of OHS interventions for companies and
their owners. There are probably some implicit social values underlying these
biases but, quite apart from the unattractiveness of using analytical methods
that mask rather than expose important equity issues, what might the relevant
criteria be for inclusion or exclusion or differential weighting? What criteria
correspond to these relevant respects? Drawing on the health care literature,
we describe several commonly adopted equity criteria.
Box 2: Horizontal and vertical equity
One
very common criterion is need. In terms of horizontal and vertical equity it
requires the equal treatment of people with equal needs, and more favourable
treatment of people with greater needs. A fundamental challenge with this
criterion is that it is far from clear how to define need. It can be defined by
ill health, which would suggest that people who are equally ill ought to be
treated the same (i.e., receive the same priority in attending to or treating
their injury or disease), and those that are sickest ought to receive higher
priority. Need might also be defined by risk exposure, in which case people
equally at risk of injury, disease or death ought to be treated the same, and
those with greater risk should be given priority.
A
key disadvantage of the need criterion is that it appears to assume that all
the conditions in question are equally treatable by health care or preventive
measures, and that all conditions or hazardous situations are equally costly to
remedy. But this is clearly not always the case. It does not make much sense to
provide equal priority for health care services to individuals with equal need
if their ability to benefit differs substantially, or if the costs of
healthcare provision are vastly different. In the context of OHS interventions,
it can hardly be appropriate to require a workplace to provide health care
services or preventive measures regardless of effectiveness or cost simply
because of equality of need define by risk exposure or rates of sickness
absenteeism. In short, the proportionality requirement implied by the criterion
of need (and the share of resources the criterion suggests that each workplace
receive) seems arbitrary and therefore inequitable.
A
second common criterion is deservedness (desert). This criterion requires that
people having equal deservedness be treated the same, and people with greater
deservedness be given higher priority. Aspects of deservedness that proponents
of this view often have in mind are lifestyle choices such as macho workplace
behaviours, smoking, drug abuse, poor diet, dangerous sports, careless and
promiscuous sex that increase exposures to deleterious health risks and the
probability of experiencing injury, disease or death. Lifestyle choices that
adversely affect health are grounds for giving individuals that make such
choices a low priority. In contrast, individuals with greater deservedness
should be given higher priority. Greater deservedness may be based on
characteristics such as clean living, higher productivity, more dependent
children, or more public service work.
There
are two critical concerns with the criterion of deservedness. First, it is
difficult to distinguish empirically between lifestyle choices and other
factors that bear on health. Second, it assumes that lifestyle differences are
avoidable rather than socially conditioned, thus making the people in question
culpable for the impact of these differences on their health. In this respect
the criterion becomes close to victim-blaming. For example, is it fair to blame
(or to discriminate against) a drug addicted youth for their poor health if
that youth had parents with similar addictions and was raised in a deprived and
marginalized household? In the workplace setting, is it fair to blame a worker
for compromising their health following a workplace accident in which the
person did not wear the appropriate safety equipment? It might have been that the
safety equipment was not provided by management, or emphasis was given to
expediency rather than safety, or that it was widely perceived that the general
culture of the organization gave safety a very low priority. Even the
apparently quantifiable criterion of deservedness based on social contribution
is difficult to measure without arbitrariness. Are claimed contributions to be
taken at face value? Can one meaningfully separate the productive contributions
made in team work? Might not even partial measures of deservingness exacerbate
rather than diminish inequity?
A
third criterion concerns the resources employed to address equity issues. This
criterion is usually presented as a strictly horizontal equity argument. It
suggests that, since all people are to be regarded as fundamentally equal, each
individual ought to have an equal amount of resources available to address
health concerns, and that the per capita distribution ought to be everywhere
the same. While the criterion is usually thought of in the context of assigning
health care budgets to regional health care providers or commissioning
agencies, it is also implicit in claims that certain workplaces, or
occupational groups, or industries have an unfair share of OHS resources.
A
primary disadvantage of this criterion is that, like the criterion of need, it
ignores the productivity of the resources expended to address health concerns.
It is difficult to justify an equal expenditure of resources in cases where the
capacity to benefit differs. For example, it would seem inappropriate to invest
an equal amount of resources in prevention in all workplaces, when in some
cases it may be very effective (and low cost) and in others quite ineffective
(and high cost). The same issue arises with resources expended for the
treatment of health care conditions arising from workplace exposures. What is
equitable about expending the same amount regardless of the injured or ill
workers capacity to benefit from it?
This
leads to a fourth equity criterion: capacity to benefit. This requires that
people with an equal capacity to benefit be given equal treatment, and those
with greater capacity be given priority. Applied to the workplace, it suggests
that people with an equal capacity to benefit health wise from a workplace
intervention ought to be treated the same, and those with higher capacities to
benefit ought to be given priority and/or have more resources expended on them.
While
the capacity to benefit criterion addresses the concern about the productivity
of resources invested in health care and prevention, it so happens that
individuals with a relatively greater capacity to benefit generally have better
health to begin with (e.g., individuals with higher education and higher
income). Hence, the application of this criterion in health care and the
workplace context would exacerbate existing health and income/wealth
inequalities. This equity criterion is a good example of how there can be
fundamental conflicts between different equity criteria.
A
fifth criterion on which to base equality is health itself. The objective of
this criterion is to achieve the greatest possible equality of health by giving
priority to those with relatively poor health. This approach was formalized in Rawls maximin principle (Rawls
1971), which we discuss in the next section. The equality of health criterion
could be implemented by prioritizing interventions based on the level of health
of individuals in different work settings (e.g., by giving higher priority
and/or investing more resources on those who are the furthest away from the
average health level of the population), or based on the level of health risk
exposure in a workplace.
A
key disadvantage of the equality of health criterion is that it suggests
expending enormous amounts of resources for very sick individuals, or those
most at risk. But such interventions may not be very health enhancing and they
might well be undertaken at the expense of interventions that would generate
much greater health gains for others. This concern is similar to that presented
in the equality of need criterion.
A
sixth equity criterion is equity of access. In health care it is often framed
as equality of access for equal needs. It would entail providing equal access
for equal needs, and priority access for greater needs. This criterion is
perhaps the most frequently encountered type of equity criterion invoked in
health care, but could also be applied to OHS interventions. For example, one
could allow for equality of access to health and safety training programs or
equality of access for worksites to resources for investment in prevention
interventions. Greater need might be defined by productivity or income, and
hence priority or faster access to health care and return-to-work services
might be given to injured workers on the grounds of their economic productivity
or to minimize compensation benefits.
Box 3: Summary of equity criteria
|
Equity Criteria
|
Horizontal equity interpretation
|
Vertical equity interpretation
|
Disadvantages
|
|
Proportionality of need
(process)
|
treat people with equal
needs the same
|
give priority to people
with greater needs
|
·
capacity to benefit may differ for similar
needs
·
cost may differ to address similar needs
|
|
Proportionality of
deservedness (process)
|
treat people with equal
deservedness the same
|
give priority to people
with greater deservedness
|
·
difficult to distinguish between choices and
other factors
·
assumes lifestyle differences are choices
·
difficult to measure social contributions
|
|
Proportionality of
expenditures (process)
|
provide an equal amount of
resources for each person
|
---
|
·
capacity to benefit may differ across
individuals
·
local price variations result in different
resources per person
|
|
Proportionality of capacity
to benefit (outcomes)
|
treat people with equal
capacity to benefit the same
|
give priority to people
with greater capacity to benefit
|
·
can exacerbate existing inequalities since
capacity is generally higher for healthier, higher income individuals
|
|
Proportionality of health
endowment (outcomes)
|
treat people with equal
health the same
|
give priority to those with
relatively poor health
|
·
maximin principle
suggests expending enormous amount of resources on the worst off
·
small gains at high cost may be at the expense
of large gains at low cost
|
|
Proportionality of access
(process)
|
provide equal access for
people with equal needs
|
give priority access for
people with greater needs
|
·
substantial resources may be expended if
access is exercised
·
capacity to benefit may differ for similar
needs
·
health inequalities may persist
·
large gains at low costs may remain untapped
|
A
disadvantage of this criterion is that it might result in high costs if many
workers exercise their right to access, yet health gains associated with access
may vary substantially. Related to this concern is that health inequalities may
persist, and there may remain many untapped gains that could be had at a low
cost.
Box 3 presents a
synopsis of the six equality criteria. The six are not an exhaustive list of
possible criteria, but are illustrative of the many and conflicting ways in
which equality may be defined. Each has disadvantages and no one is best for
all decision contexts. Ultimately, a process in which stakeholders and decision
makers participate in the assessment of equity implications of an evaluation
might result in the most appropriate choice of equality principle to adopt for
a particular situation.
Efficiency versus equity
There is a fairly robust tradition
in both the economics and the philosophical literatures that casts efficiency
and equity in competing roles. While it is undoubtedly true that conflicts can
arise, it is helpful to bear in mind two considerations:
·
the
tension between rival equity criteria is greater and often harder to resolve
than the tension between equity and efficiency;
·
the tension between equity and efficiency arises
largely because efficiency requires the aggregation of individual consequences,
and if this aggregation is undertaken without thought being given to its
distributive equity implications, it is highly likely that the efficient
alternative will appear inequitable (Culyer 2006).
The tension between rival equity
criteria may be hard to resolve, but it can at least be elucidated by
identifying and clarifying the criteria under consideration. In the context of
a specific evaluation, if there is a concern about the relevant criteria to be
considered, then offering stakeholders and decision makers a list of
possibilities as presented in Box
3 may be a useful point of departure.
The apparent tension between
efficiency and distributive equity can be illustrated by an example from health
technology assessment. A typical evaluation would consider the health
consequences of alternative treatment options measured in Quality-Adjusted
Life-Years (QALYs). The objective may be specified as selecting the technology
with the highest incremental cost-utility ratio from a set of possible options.
Total health consequences would be measured as the net present value of a
discounted stream of future QALYs and added across the individuals who are
predicted to benefit. Simple addition within and across individuals assumes
that the social value of an additional QALY is the same regardless of who
receives it, and how many any one individual receives. Essentially, all QALYs
are given equal weight.
Should it turn out that QALYs are
thought to be of different value depending on who receives them and/or how many
are received by any one individual then the efficient alternative might be in
conflict with the relevant equity criterion. The
conflict disappears if appropriate weights are attached to QALYs instead of
assuming equal value. Weights might be based on generic characteristics of
recipients such as age, gender, and number of QALYs received (we discuss equity
weights in greater detail later in the chapter). Alternatively, the efficiency
analysis based on the assumption of equal value of QALYs could be explicitly
presented as provisional, with the ultimate decision to be taken after a
decision-making body gives due consideration to the equity implications of
alternatives in addition to the provisional efficiency analysis. The key point
is that both efficiency and equity must be considered in tandem, with neither
trumping the other.
Perhaps the principal lesson from
this brief review of equity criteria is to emphasise the importance of being
clear about the underlying equity principles being invoked when assessing the
distributive equity of alternatives. As is apparent in the above descriptions
there are multiple concepts of equity, some of which are compatible and others
which are not. Many discussions of equity are typically fraught with
generalized slogans and particular interest groups will tend to select those
that most favour their own interests. In order to enhance the clarity of
analyses of the equity implications within the context of economic evaluations,
we suggest considering, consulting and reporting the answers to the following
questions:
·
What are the appropriate relevant respects
(criteria) to be borne in mind in the situation at hand?
·
Are the equity criteria under consideration
appropriately distanced from the particular interests likely to be affected by
the intervention?
·
Are the equity criteria addressing horizontal or
vertical equity?
·
Are the equity criteria addressing process such
as access or exposure (procedural justice) or outcome/consequences such as
better health (distributive justice)?
Equity constructs
In
what follows, we review several well-know equity constructs found in the
literature. Some have been considered in the economics literature, and
specifically in health economics, whereas others come from other disciplines.
Some approaches provide guidance on how to embody equity in a decision-making algorithm, as through the use of
weights to adjust health or utility values based on the characteristics of
recipients. Others provide guidance on how equity concerns can be incorporated
alongside evidence into the decision-making process itself in order to afford
an opportunity for decision makers to delve more deeply by considering the
individuals that are likely to gain or lose from an intervention and the nature
of their gains or losses. Decision makers may also consider how best to manage
the introduction of a worthwhile intervention that has both gains and
uncompensated losses in light of equity concerns. Our emphasis is on providing
appropriate information to decision makers rather than deciding precisely how
equity is to be embodied in the analysis.
The fair innings approach
Williams (1997) fair innings
approach was developed in the context of the UKs National Health Service (NHS)
to address issues of distributive equity, specifically as they related to
vertical equity. The approach assumes that one of the objectives of the
NHS is to reduce inequalities in peoples lifetime experience of
health. Age matters in two respects. First, it affects peoples
capacity to benefit and therefore places older people at a general
disadvantage if another objective is to maximise the (unweighted)
benefits of health care. Second, older people are more likely to
have had fair innings in terms of experiencing many years of healthy life, and
this places them at a lower priority based on the notion of minimising differences
in lifetime health. Williams argued that it would be equitable to provide small
benefits to young people even if in so doing the elderly were denied
large benefits, provided that the young recipients had a low probability of
achieving a fair innings. The approach does not necessitate young
people having absolute priority for benefits compared to older
people. Rather, it simply means that their health benefits are given greater
weight. Applied to economic evaluative methods, the fair innings approach
suggests that generic characteristic be used to weight benefits (and possibly
costs) differently. Age would be the principal characteristic to consider,
though other characteristics might also be used in the developing weights. In
all cases, the following three factors should be considered:
·
Is
the ethical argument for weighting benefits differently based on a recipients
characteristics acceptable in the context of the given evaluation?
·
Is
there an acceptable method for identifying or developing appropriate weights?
·
Are
the issues involved best addressed by weighting benefits or through a
deliberative approach that would allow for additional evidence to be considered
in the decision-making process?
The World Health Organization
developed a weighting system based on age for use with a health outcome measure
known as Disability Adjusted Life Years (DALYs) to measure the global burden of
disease (Murry and Lopez 1996). DALYs measure the
health gap due to injury, disease and premature mortality based on a gold
standard of a full and healthy life of 80 years for men and 82.5 years for
women. Weights were developed for DALYs based on the notion that years of
healthy life in early adulthood are worth the most to society. DALYs during the
early years of life from birth are given lesser weight but increase
substantially in the years to early adulthood and decline gradually thereafter
into old age.
Justice as fairness
Rawls (1971) developed a theory of
equity that has been particularly influential for health economists, even
though he explicitly excluded health and health care in his analysis of justice
as fairness. Rawls proposed a hypothetical situation for assessing equity
issues in which individuals making decisions are shrouded by a veil of
ignorance such that they have no knowledge about their own personal
circumstances or position in society. Such a veil provides a distance between
self interest and considerations of equity. Rawls conjectured that such an
approach would result in an agreement on two basic principles of fairness:
·
Basic
liberties (such as the rights to vote, freedom of speech, and the right to own
property) ought to be both equally distributed and as complete as is consistent
with equality; and
·
Primary
goods (such as basic liberties, income and wealth, position of responsibility,
and respect) should be distributed such that only inequalities that were to the
benefit of the least advantaged people would be permitted. This criterion is
known as the maximin principle.
Primary goods include attributes
essentially determined by the interactions in human societies, but not natural
goods such as health. Primary goods are a means to an end, a means to
attaining welfare. Rawls excluded health from the list of primary goods because
health is an end in itself, because it is determined largely by nature, and
because he felt that the application of the maximin
principle to health could lead to large amounts of health care resources being
devoted to the health of people who would gain little from it, possibly at the
expense of driving others into poverty.
Equity and capabilities
Sen (1980, 1993) argued that
non-utility characteristics often provide better grounds for assessing the
equity implications of alternative social states than utility and welfare.
According to Sen, a particularly important class of
non-utility information is peoples basic capabilities. These capabilities are
ones that enable people to engage in activities that are important to them,
such as working, using leisure time, community involvement, and living a
healthy life. Equity concerns should thus focus on the distribution of basic
capabilities. The approach suggests that equity is about moving society towards
a more equal distribution of capabilities. Sen
suggested that many basic capabilities can be measured as levels of
functioning. This is certainly true for health.
The basic capabilities approach is
extra-welfarist in that it goes beyond the evaluation of human welfare and its
distribution in terms of individual utilities. The approach does not provide an
algorithm. Its value lies in the framework it provides for thinking about
equity issues. It leaves a good deal to the discretion of analysts, such as
determining what counts as basic capabilities in health and in a workplace
context, how they are to be measured and weighted. One approach for the
economic analyst might be to create a process for reasoned agreement with stakeholders,
bearing in mind the specific decision context.
The rule of rescue
The rule of rescue approach to
equity consists of an injunction to rescue identifiable individuals in
immediate peril, regardless of cost. The
plausibility of the rule is well-expressed in the following quote (Jonsen 1996,
quoted by Cookson et al. 2007):
Our moral response to the imminence of death
demands that we rescue the doomed. We throw a rope to the drowning, rush into
burning buildings to snatch the entrapped, dispatch teams to search for the
snowbound. This rescue morality spills over into medical care, where our ropes
are artificial hearts, our rush is the mobile critical care unit, our teams are the transplant services.
The appeal of the rule lies in the
heroics expressed in the rescue process. The downside is that though an intervention
may rescue people facing imminent death, it may give them only a small
increment in extra life. Furthermore, the cost of funding the rescue technology
may divert resources away from other activities that provide substantially
greater benefits to others. Essentially, the rule of rescue focuses on the
benefit to one group (whose identities are usually known) and ignores the cost
to others (who are probably anonymous potential beneficiaries of forgone
opportunities). There is an implicit interpersonal comparison which values the
benefits of one group over those of another. Concern for identifiable
individuals in immediate peril unambiguously implies less concern for
unidentifiable individuals in future peril. Such discrimination, when it is
seen for what it is, seems intuitively unpalatable. Though it is based on a natural human
expression of good will, it entails gross inconsistency in the way it treats the
value of resources (Cookson et al.
2007). The approach is not the same as having a concern for the severity
of a current health condition or risk exposure in a working environment.
Rather, it would suggest providing increases in safety of a value that need not
be compared with its cost in order to favour identified individuals at the
expense of the unidentified.
Libertarianism
Some
procedural approaches operate at a very broad level. Libertarianism in its
classical forms (e.g., Locke 1967) or its contemporary version (e.g., Alchian 1965; Nozick 1974)
accords a minimal role to the state, based on the premise that there is little
justification for any regulation beyond that required to operate a system of
exchangeable private property rights. There is no scope for agencies to promote
or regulate efficiency, equity or health and safety. No individuals right,
small or large, should ever be sacrificed for any other end, including the
rights of other. This approach is tantamount to denying the legitimacy of any
concept of equity, unless outcomes are automatically defined as equitable if
they are a product of an equitable process which, according to libertarianism,
would exist in a market uncluttered by regulation. The pure form of
libertarianism plainly implies that allocative
decision-making tools such as economic evaluation are not liberal. However,
provided that the stakeholders in any given practical situation in which an
economic evaluation is being planned can agree that the existing rights and
entitlements of stakeholders are satisfactory, it is possible that a case can
be made for a consultative process that would determine the methods to be used
to choose the optimal set of health and safety interventions and how evidence,
and what kind of evidence, would be incorporated into the process.
Accountability
for reasonableness
A
much less extreme approach than libertarianism is that of accountability for
reasonableness (Daniels and Sabin 1998; Daniels 2000). This approach
incorporates the fact that there is often reasonable disagreement about
relevant equity criteria. The approach provides some principles of a legitimate
and fair process for making decisions without needing to specify any specific
outcome. Key elements of a fair process include transparency about
the grounds for decisions, appeals to rationales that all can accept
as relevant to decision making, and procedures for revising
decisions in light of challenges to them. Together these principles
insure accountability for reasonableness. Box 4 provides an example of an
application of this approach.
Box 4 Application of accountability for reasonableness
Deliberative processes
A deliberative process is characterised
by a careful, deliberate consideration and discussion of the advantages and
disadvantages of various options in an effort to assist people with making a
decision (Hajer and Wagenaar
2003). A deliberative process is used to elicit and combine various types of
evidence. A deliberative process integrates scientific analysis and social
context, with stakeholder or lay public views elicited
through consultation and participation. However, a deliberative process is
different from a consultative process in that it requires participation rather
than simply consultation (see Box
5 for an example of a consultative process that was not a
deliberative process). Employing a deliberative process increases the
likelihood of achieving a sound and acceptable decision (Daniels 2000). If
properly executed it will be more comprehensive in the relevant issues
embraced, more consistent in the way they are embraced and more engaging of the
people affected by the outcome than a closed-door or ad hoc process (Culyer and Lomas 2006).
Box 5: Example of a consultative process
The
following conditions are hypothesized to be those under which a deliberative
process is most likely to be warranted:
·
evidence from more than one expert discipline is
involved;
·
evidence from more than one profession is
involved;
·
stakeholders have conflicting interests;
·
there are technical disputes to resolve;
·
evidence may be scientifically controversial;
·
evidence gathered in one context is to be
applied in another;
·
costs and consequences extend beyond the
conventional boundaries of business planning;
·
there is substantial uncertainty about key
values and risks that needs to be assessed and weighed;
·
there are social and personal values not taken
into consideration in the scientific analyses;
·
there are issues of equity involved;
·
there are issues of implementability and
operational feasibility; and
·
a wide public and
professional ownership is desired.
As
is apparent, equity is one of the items on the list, and it is often one of the
most important and intractable factors under consideration. A deliberative
process is particularly useful when equity is a central concern in a decision
because of the uncertainty surrounding the appropriate equity criterion to
adopt, the general absence of quantitative data to inform equity issues, and
the uncertainty about how to trade off equity against other considerations such
as efficiency, implementability and manageability.
Equity and incidence
A matter that may have considerable
implications for judgements about equity is the divergence between the initial
and final incidence of costs and benefits. The most common application of the
theory of incidence in economics is in the field of taxation, where the initial
incidence of a tax change is compared with its final incidence or burden after
all market adjustments in response to the change have been completed.
As
an example, consider the kind of effects that might follow the adoption of a
costly new intervention to enhance worker safety. The initial incidence of
costs will reside with the firm as new equipment is acquired, old equipment
modified, new training schemes deployed and new management structures created.
However, in the medium to long term the combination of a safer working
environment and shifts of the skill mix and other substitutions may cause wages
to decrease since, all else being equal, a safer environment will generally
result in a lower wage (higher wages normally compensating to some extent for
higher risks). The effects on the production side may affect overall marginal
costs and generate a change in the price of the products produced, which in
turn may generate a change in the amount demanded in any time period. It is
possible that what was initially a cost to the firm turns out to be no burden
at all, with the costs falling on consumers, or workers or both via higher
prices and lower wages. However, the working environment will still be safer
than before the intervention, which is of benefit to workers. Moreover, if
greater safety has positive productivity effects, it may translate into an
increase in wages and profits.
The
implications for assessing the equity aspects of OHS interventions should be
apparent: if it is possible for the initial incidence of the costs or benefits
of any change to be shifted to others, then any assessment of the equity of the
change that fails to account for this would be flawed. How significant such
effects are is an empirical matter. Whether it is worth modeling
these shifts to estimate their magnitude will be a judgment that should be
based on factors such as:
·
How far reaching the intervention is in terms of
the number of workers and firms affected. The greater the scope of the
intervention, the more likely it is that incidence will be shifted in ways that
might affect judgments of equity.
·
The size of the firm level intervention in terms
of cost, health and productivity effects. A modest intervention will generate
smaller shifts.
·
The competitiveness of the labour and product
markets in question. Less competitive labour and product markets will have
smaller elasticities, and hence lesser responses.
·
The speed of implementation of the intervention.
The costs of slow or gradual implementation tend to be lower than fast
implementation and shifting of burdens will take place over a longer period of
time.
·
The effectiveness of the intervention. A less
effective intervention will generate less scope for shifting.
Recommendations
·
Identify
the relevant stakeholder groups who may gain or lose from an intervention and
provide an analysis of the gains and losses by group.
·
Ensure,
so far as possible, that the idea of equity is distanced from the self-interest
of any participating stakeholder group.
·
Determine
whether the equity issues are horizontal, vertical or a mixture of both.
·
Clarify
the relevant respect(s) or criteria in terms of which individuals and groups
are to be differentiated.
·
Decide
whether the process of decision making or of subsequent roll-out of the
intervention is itself a part of the equitable solution.
·
Consider
whether equity is better treated in an algorithmic fashion (e.g., by weighting
various elements of a calculated cost-effectiveness ratio) or by
consultation/deliberation of some sort.
·
Consider
differential weights for costs and consequences accruing to different
individuals and groups. Be clear about their calibration and justification.
·
Explore
the possibility of determining equity weights through sampling relevant
sections of the population.
·
Consider
whether, should a consultative route be followed, it be merely consultative or
also deliberative.
·
Be
on guard for special pleading masquerading as the rule of rescue.
·
Consider,
where appropriate, adjusting for the difference between the initial and the
final incidence of costs and consequences.
Bibliography
Alchian A (1965). Some economics
of property rights. Il Politico, 30, 816-29.
Cookson R, McCabe C, and Tsuchiya A (2007). Public health care resource allocation and
the rule of rescue. University
of Sheffield Health
Economics and Decision Science Discussion Paper 07/04.
Culyer AJ (2006). The bogus
conflict between efficiency and equity. Health Economics, 15, 1155-8.
Culyer
AJ and Lomas J (2006). Deliberative
processes and evidence-informed decision-making in health care do they work
and how might we know? Evidence
and Policy, 2, 357-71.
Daniels N (1985). Just health care. Cambridge University
Press, Cambridge.
Daniels N (2000). Accountability
for reasonableness. British
Medical Journal, 321, 1300-1.
Daniels N and Sabin JE (1998). The ethics of accountability in managed care
reform. Health Affairs, 17, 50-64.
Dolan P and Olsen JA (2002). Distributing health care: economic and ethical issues. Oxford
University Press, Oxford.
Donaldson C,
Gerard K, Mitton C, Jan S, and Wiseman V (2005). Economics
of health care financing: the visible hand, (second edition). Palgrave
Macmillan, Houndmills.
Folland S, Goodman AC, and Stano M (2004). The economics of health and health care, (fourth
edition). Pearson Prentice Hall, Upper Saddle River NJ.
Garland MJ (1992). Rationing in public:
Oregons priority-setting methodology. In MA Strosberg, JM Wiener, RB Baker and IA Fein, ed. Rationing Americas medical care: the Oregon
Plan and beyond: papers, pp 37-59. Brookings Institution,
Washington, DC.
Hajer MA and Wagenaar H (2003). Deliberative policy analysis: understanding governance in the network
society. Cambridge
University Press, Cambridge.
Hausman DM
and McPherson MS (2006). Economic analysis, moral
philosophy, and public policy, (second edition). Cambridge University
Press, Cambridge.
Locke (1967). Two treatises on civil government. P Laslett,
ed. Cambridge University
Press, Cambridge.
McGuire
A, Henderson J, and Mooney G (1992). The economics of health care: an introductory text. Routledge, London.
Mooney G (1992). Economics, medicine and health care.
Harvester Wheatsheaf, Hemel Hempstead.
Murray CJL
and Lopez AD (1996).
The global burden of disease: a comprehensive assessment of mortality and
disability from diseases, injuries and risk factors in 1990 and projected to
2020. In Global burden
of disease and injury series, (volume 1). Harvard
University Press, Cambridge.
Nozik R (1974). Anarchy, state and utopia. Basic Books, New York.
Plant R (1991). Modern political thought. Basil Blackwell, Oxford.
Rawls J (1971). A theory of justice. Harvard University
Press, Cambridge.
Sen A (1980). Commodities and
capabilities. Oxford University Press, Oxford.
Sen A (1993). Capability and well-being.
In M Nussbaum and A Sen, ed.
The quality of life,
pp. 30-53. The Clarendon Press, Oxford.
Wagstaff A and van Doorslaer E (2000). Equity in health care finance and delivery. In AJ Culyer and JP Newhouse, ed. Handbook of health economics, pp. 1803-62. Elsevier, Amsterdam.
Williams A (1997). The rationing debate: rationing health care
by age: the case for. British
Medical Journal, 314, 820.
Williams A and Cookson R (2000). Equity in health. In AJ Culyer and JP Newhouse, ed. Handbook of health economics, pp. 1863-1910. Elsevier, Amsterdam.
What is a little more health and safety worth?
Anthony
J. Culyer, Benjamin C. Amick III, Audrey Laporte
The
innocent-sounding question posed in the title of this chapter is our way into
these issues. It is meant to lead us into an exploration of the issues that
arise in evaluating the effectiveness and cost-effectiveness of workplace
interventions to promote health and safety (note that some researchers may
consider that cost-effectiveness already includes effectiveness, but it is a
distinction commonly made and familiar to many people-- see Box 1 for some basic definitions).
Box 1: Some basic definitions
Ends and
means
Our
thesis question may appear odd to those in the world of workplace health and
safety who are not economists. After all, better health seems a reasonable
objective for individuals and governments to aim at. It is an end. But safety at work is a means one
of many means to the end of better health. More precisely, the means are the
methods by which risks to health in the workplace are managed; so the means are
the instruments, policies, workplace interventions and the like that are
adopted in workplaces and which reduce the probabilities of events occurring
that are harmful to health. These means are at best intermediate outcomes that
lie on the road to the more ultimate outcome, better health. Hence, the
worthiness of any risk reduction is presumably to be measured in terms of its
impact on health. Considering the value of both health and safety is to invite
the danger of double counting (see Box
2 on forms of double counting). It is health that is to be
valued. The value of safety depends primarily on the value of the incremental
health it enables.
But
means and ends can become intertwined. Less risk, independent of any health or
other consequences, may be preferred since people are generally risk-averse.
Just feeling more secure is a benefit. It is not a health benefit in the
conventional sense of what health is, but it does affect a persons welfare.
Box 2: Forms of double counting
One
might focus on consequences other than health. For example, an employer may implement
engineering controls in order to eliminate a safety hazard and increase
productivity without considering the direct value of health benefits. This
suggests another perspective, one that does not view health as the ultimate
objective but, rather, increased productivity. From such a perspective the
means remain the reductions in risk, but the end is increased output, something
to which it is relatively easy to attach a monetary value. Of course, in many
cases health and safety interventions enhance both health and productivity.
Notwithstanding
the fact that safety is in many cases a means, we have identified three ends
associated with resource investment in health and safety that are of value to
society: improved health, the inherent value of greater security, and enhanced
productivity. Resource use may be directly linked to improved health, as is the
case with health care services. In some cases productivity effects (note that
we use the terms consequence, benefit and effect interchangeably) may
arise through the impact of resources on health, as when effective disability
management enables a safe return to work sooner than would otherwise have been
the case, or when sickness absences are reduced through safer working
conditions. In other cases, productivity may be affected directly through
workplace safety enhancements. There may also be a link from productivity
increases to health increases. These various pathways are depicted in Figure 1
below.
Figure 1: The relationship between
productivity and health
Two
types of complexity are involved in the foregoing. The first is a complexity
arising out of the need to determine what consequences ought to be considered.
Three beneficial consequences have been mentioned and depicted in the diagram,
but what other possible candidates are there and how are they to be measured
and compared? Furthermore, consequences to whom? Is it
only those to workers, or ought we also to consider workers families and
dependents, owners of firms, insurance agencies, and consumers of the outputs
produced by the workplaces in question? And when we use the word ought, what
are the ethical criteria to which we are appealing? These are lofty questions
which we try to address in what follows in this chapter. The second complexity
concerns the pathways of causation and interaction between means and ends, and
how some ends can even, as we have seen, in turn become means.
These
complexities are familiar challenges to economists. The first set involves a discussion
of human welfare, its measurement, its distribution, and its aggregation. The
second involves the production function, or in other words, the analysis of the
ways in which inputs are transformed into outputs and how feedback effects are
taken into account.
Cost-effectiveness
analysis (CEA) is something of a hybrid of the two kinds of complexity. It
usually considers both benefits and opportunity costs as being dependent on
peoples preferences and it tends to be action-oriented by focusing on the use
of technologies to change workplace practices, or on the technologies of health
care. The notion of technology can be very broad: a drug, a guard on a machine,
non-slip surfaces, an OHS management system, a modification to a health
insurance system such as the introduction of a no-fault system, or the
introduction of experience-rated employers premiums. In effect, the
technologies that are evaluated in cost-effectiveness analysis are ways of
doing things.
The
philosophical framing of economic evaluation
The
approach economists generally adopt is known as consequentialism
in philosophical writing. Consequentialism is a class
of ethical theories sharing the view
that the morality of actions or arrangements is to be judged by their
consequences. Consequentialism is often
contrasted with deontological moral theories which hold that the morality of
actions and arrangements is to be judged in terms of duties and rights. Essentially, consequentialism
is the notion that the outcome ought to justify the means. The most famous
approach within this class is called act utilitarianism (see Box 3).
Box 3: Utility theories
Consequentialism may not be a useful approach in some
decision contexts. For example, considering only costs and consequences is
certainly not the only way of evaluating the pros and cons of alternatives for
a disciplinary case. One may want to take account of the motives of a person
who might be subject to disciplinary action. There are other objections to consequentialism. The most common one comes in the form of
a dogmatic statement, the end can never justify the means. But if an end
cannot justify a means, then what can? It may be that a particular end does not
justify a particular means, and it may also be that some means are so awful
that they cannot be justified by any end. But, if there is a justification for
adopting any particular means of advancing safety at work, we adopt the working
hypothesis that it lies in its consequences for workers health, for their
families welfare, for productivity, for the need for compensation and, indeed,
for the well-being of any and all those affected by it.
The
question of perspective
There
is a value judgment in the foregoing. We have asserted that the justification
ought to be in terms of the well-being of any and all who are affected by it.
This is to adopt a particular perspective, commonly termed the societal
perspective. In the world of affairs this is not always, and perhaps rarely,
the way in which decisions are reached. In some workplaces, the decisions will
be taken by managers who see their prime responsibility as being to serve the
interests of owners, so that interventions having benefits that accrue
exclusively to workers will not gain acceptance. Workers, on the other hand,
may perceive only the benefits that accrue to them, fight to achieve them, and
ignore the disadvantages that fall on the owners. Plainly, the distribution of
costs and consequences affects behaviour, attitudes, and the chances of success
in advocacy. In practical politics these things matter. But they also matter
when a deeper ethical question is addressed: what policies, controls,
regulations, interventions, inspections, penalties and rewards and the like ought to be introduced? Or put another
way: what is the value of a little more safety in the workplace, and of value
to whom?
Another
notable feature of the question in the title of this chapter is that it needs
to be asked at all. One might have expected that the question of the
worthwhileness of health and safety would have been resolved long ago, or at
least that the methods by which an answer is to be reached, and the principles
underlying those methods, would have been long-since settled.
The
answer may lie partly in the inherent difficulty of conceptualizing and
measuring the effects of workplace health and safety interventions. Conducting
experiments that control for confounders in hugely complex work situations is
virtually impossible. Another part of the answer lies, we conjecture, in the
way that the academic disciplines that are closely engaged in the OHS field
have been applied. It seems that many analysts amongst the practitioners of the
various clinical, statistical, public health and social scientific fields
engaged with workplace health and safety issues view more health and better
safety as always preferred, regardless of what they may cost. It is really only
a question of figuring out what works. There has been, we detect, a tendency to
see things through the lenses of the workers. Moreover, scientists have often
not set out to refute hypotheses about the effectiveness of the means they
adopt or recommend, but rather have focused on proving them, thus reversing the
standard scientific and statistical approach to hypothesis testing (We are not
intending to imply support for naïve falsificationism
here). In opposition are views that may be more characteristic of employers,
for whom the lens of worker welfare may seem less relevant, unless there were
some indirect effects on profitability, and for whom the bottom line and
managerial convenience may be the dominant considerations. Neither set of
attitudes is to be despised, but a truly analytical approach to addressing the
question of the social value of greater workplace safety and better worker
health must find some way of escaping sectional bias.
Scylla, Charybdis and a safe passage
There
are three commonly used approaches to evaluating health and safety procedures.
Navigating around the first two, we feel much like Odysseus sailing around
Scylla and Charybdis, the rocky reef and whirlpool in the straits of Messina. In what follows we outline each of
the three approaches, explain the disadvantages of the first two, and describe
our reasons for preferring the third. The three go by the following names: the
perfect market approach, the human capital approach and the decision-maker
approach.
The
perfect market approach
The
perfect market approach is premised on the notion that markets function
reasonably efficiently, thus rendering formal evaluation of the effectiveness
of health and safety procedures unnecessary. The general objective and ultimate
criterion for deciding worthwhileness embodied in this approach is the
standard economic maximand: the sum of the expected utilities of all affected
persons. This leads one to the Panglossian conclusion
that the world is best left as it is (Doctor Pangloss
was Candides mentor, for whom the world today was
the best of all possible worlds). Workers and employers are best left free to
negotiate mutually agreeable terms of employment which cover wages, salaries,
other benefits and workplace safety. Both sides can shop around costlessly, according to their preferences and, in
particular, their attitudes towards risk, in order to find a suitable matching
of person to job and job environment. Those who are risk-averse will seek safe
environments or require compensation for working in riskier workplaces, and
trade off the positive and negative aspects of the various offers of labour or
employment available. All other things being equal, safer environments will
tend to be associated with higher priced products and lower real wages than
less safe environments, as there will be no necessity for employers with safer
environments to offer compensating wage differentials. In equilibrium, all pros
and cons will have been duly weighed within the overall resource constraints of
the economy and safety and health will have been optimized, along with
everything else.
In
such a vision of the world, neither the interventionist policies we commonly
observe, nor the normative economic calculations that can underpin them, are
necessary. Nor even are voluntary collective actions by firms such as the
Voluntary Protection Programs in the USA (Rees 1988). A risk that is voluntarily adopted after whatever
compensation is agreeable to the consenting parties is a socially acceptable
risk. It is the best that can be done in a world in which risk of injury and
disease is generally to be avoided but is in practice costly to avoid.
In
general, the theory of compensating wage differentials predicts that jobs
requiring a higher level of education will, other things equal, pay more than
those requiring a lower education in order to compensate employees for their
investment in additional education. Jobs associated with higher risk of injury
or disease will, other things equal, pay risk-averse workers more than they
could earn in other safer jobs for which they are qualified, thus compensating
them for the greater likelihood that their working life may be shortened, as
well as any financial and psychic costs they might suffer due to injury or
disease.
Compensating
wage differentials must be offered by employers who save on health and safety
costs by offering less desirable work environments. Such differentials enable unpleasant
but necessary jobs to be done. Employers who improve the health and safety of
work environments do not have to offer compensating wage differentials, but
they incur the costs of the improved work environments. Whether environmental
changes at work dominate over wage adjustments will depend partly on the
relative costs to the employer of changing work environments and the
anticipated responses of potential workers to these changes and any changes in
pecuniary offers.
The
extent to which markets generate the desired results depends on the efficiency
of the matching process between workers and jobs in the economy. John Stuart
Mill, the great utilitarian, observed at the turn of the 20th
century that there were imperfections in the market which often resulted in the
least pleasant jobs also paying the lowest wages under circumstances which
could only implausibly be interpreted as offering a net compensating advantage
of any kind (Mill 1965). He also noted that significant unemployment would
constrain workers ability to negotiate higher wages or to reject job offers.
Mill further argued that people from marginalized groups, such as immigrants or
poor and ill-educated people could be ghettoized into the least desired
employment strata within the labour market, leading to an over-supply of such
people in competition for the least desirable jobs.
The
compensating wage differential model assumes free and complete information on
the part of workers and employers. However, if workers are unable to assess the
risk of injury or disease accurately, they may not negotiate a sufficiently
high wage. While there is some evidence to suggest that workers are fairly good
at assessing risk of death, they are less able to assess the risk of chronic
disease, or acute events, such as injury arising from slips and trips on shop
floors (Dorman 1996). Supervisory and workgroup relationships may lead workers
systematically to over- or under-estimate the significance of the various job
attributes. While workers might over time acquire a good perception of the
bundle of job characteristics, the threat of moving to another position if wage
compensation or other adjustments in the package were not implemented may be
weakened and this weakness can be reinforced if health, pension, seniority and
other benefits are at risk of being lost. Hence, the high costs of changing
jobs can impede the effective working of the market mechanism. High rates of
staff turnover are also costly to employers, since they may lose workers in
whose skills they have invested. They will also incur hiring costs and may
incur short-term losses in productivity.
Externalities
are another source of market imperfection (see Box 4 for a definition) Many
aspects of working conditions are external to the decision makers in that they
affect third parties either financially, physically or psychically. For
example, Leigh et al. (1996)
estimated that workers compensation insurance premiums paid by employers
represents only 11 percent of the costs of occupational injury and disease in
the United States, the remainder of the costs fall to workers and taxpayers.
The total economic burden is estimated at around three percent of Gross
Domestic Product, but only 10 percent of this burden is borne directly by
employers. When external costs are added to internal costs, it amounts to what
economists call social cost. Yet, it does not follow that the activity which
generates external costs ought to be eliminated, nor does it follow that
externalities should be eliminated should there be ways of reducing them.
Box 4: Externalities
The
optimal social adjustment will be one that induces the firm to act as though it
recognized the external cost so as to reduce the activity rate to that at which
the marginal social benefit equals the marginal social cost. In the case of
reducing the externality by other methods, the principle is again that the
optimal investment is that at which the social cost of reducing the risk of
harmful events is set equal to the best estimate of the social benefit from it,
i.e., the benefit to workers plus that accruing to the externally affected
parties.
The
important logical implication of this is that, because there is a cost to
reducing harm, it will generally be the case that there is an optimal degree of
reduced harm which falls short of complete elimination. Economic analysis
treats the benefits from hazard reduction in the same way as it treats other
benefits. The art therefore lies in judging the point at which reducing a
hazard costs more than the reduction is considered to be worth. This leads us
to the critical issue of perspective. One needs to consider whose costs and
benefits matter. In turn this leads us to the issue of distributive justice or
equity, a topic we return to later.
The
absence of full employment, imperfect information, lack of perfect labour mobility across jobs, and the existence of
externalities suggests that the market, left to its own devices, will not yield an optimal level of
compensation for risk and therefore workers will face a higher than optimal
level of risk. This discrepancy provides the basic case for government
intervention through workplace health and safety regulation, imposition of
minimum OHS standards, education and public information programs, and
evaluative research including the use of analytical methods of assessing risks
to health, the social significance of such risks to employers, workers, their
families and the wider community, the availability of technologies through
which such risks might be reduced, the costs of implementing such technologies
and the distribution of those costs across employers, employees and the wider
community.
There
is also the issue of equity, which is related to the fairness of the initial
distribution of wealth and power and the advantages and disadvantages that
result to various players in the labour market. Many social inequities are
multiple. Health is systematically correlated with wealth, as it is to income.
In general, the least well-off financially are also the least healthy and least
educated. They are also often the least empowered and organized. Regulatory and
other interventions have often been applied on these grounds alone, regardless
of the foregoing efficiency considerations outlined in this section. So even if
the market actually was perfect, its outcome may well not be regarded as
equitable. Those most at risk would in general be the poorest paid, the least
skilled and least educated. The pay-off to investment in safety as seen by
managers would rise in proportion to the productivity of the employees most
affected, so safety investments that benefited the rich would dominate over
those that benefited the poor. Such an outcome would violate the most basic
principles of horizontal and vertical equity: that people who are alike in
relevant respects ought to be treated alike and those who are not alike in
relevant respects ought to be treated unequally in relation to their relevant
differences. That is, unless one is prepared to argue that productivity
differentials are morally relevant aspects that justify such discrimination.
Dismissing
the perfect market line of thought will tend to also require dismissing benefit
estimation techniques based on market behaviour. This is particularly the case
in cost-benefit studies that use estimates of, for example, willingness to pay
for reductions in risk of injury or death (e.g., Gegax
et al. 1991; Moore and Viscusi 1988) or that use observed wage differentials
across employments judged to be similar in most respects, except for the risks
to which they expose workers, in order to estimate the cost of safety (e.g.,
Rosen 1986; Knieser and Leeth
1991). These are vulnerable to the same criticisms on the grounds of both
efficiency and equity. The occasions when they are sufficiently immune to such
objections always need careful assessment. In general, we think that the usual
presumption has to be that the distortions are large and significant. So it is
the use of market-based, benefit estimation techniques, rather than their
rejection, that needs explicit justification on a case by case basis.
That
was our Scylla. If it can be skillfully sailed
around, the would-be evaluator is likely to be confronted by our Charybdis: the human capital approach.
The
human capital approach
The human capital approach
dates back to the earliest attempts at applied economics with William Petty
(1691) and William Farr (1853). Petty discounted estimated wages to infinity to
compute a capital value, while Farr discounted the difference between future
income and an estimated cost of future maintenance, adjusted for the
probability of death (for details on discounting see Chapter 12). That,
essentially, is the approach adopted today by those using the human capital
approach such as Health Canada
(1998). It is, to put things rather sharply, tantamount to treating humans as
though they were carthorses. They are good only for what they produce, after
deducting what they cost in fodder and watering (for details on this criticism,
see Pritchard and Sculpher 2000). The approach neglects any benefit to
individuals that is not work-related, as for example, the direct benefit of
being free from pain, or not depressed, or not severely stressed, or able to
move about. It neglects the value to individuals of leisure time, and it also
fails to consider any external valuations of peoples time, such as valuations
by their families and friends.
The method is particularly
vulnerable to equity objections. If one persons human capital is worth twice
that of another, then it will be worth expending twice as much to avoid losing
a certain fraction of it. So those who have expectation of monetarily
productive life will have further benefits heaped upon them in the shape of
safer workplaces and better rehabilitation.
Of further detriment to the
approach is that it is not grounded in any modern welfare economics theory. The
conventional neoclassical position is that the appropriate valuation of a
reduction in the probability of loss of life is a persons willingness to pay
for such a reduction. Although subject to the same objections on the grounds of
equity as the perfect market method, it is less susceptible to the efficiency
objections provided that the willingness to pay can be obtained under
appropriately controlled experimental conditions, and provided that external
effects are taken into account (Jones-Lee 1989; Jones-Lee et al. 1985). The obvious alternative to willingness to pay to
avoid a harm is willingness to be compensated for
accepting it, but this too is not captured by the human capital approach.
Matters
become more complicated if the maximand is more comprehensive. For example,
estimates of the benefits over a working lifetime of a workplace safety
intervention will underestimate the total productive value of a life by
assigning a zero worth to childhood and retirement. If averted productivity
losses are simply added to other types of estimates, such as averted losses of
health and the averted costs of health care, there is the risk of serious
double counting. Depending on the construction of a health outcome measure, the
value of work and its contribution to ones standard of living over time will
already be embodied in the measure. If already included, the only productivity
component that ought to be added is the friction cost associated with replacing
a worker such as delays in replacement, cost of recruitment and training, etc.
(Koopmanschap et
al. 1995; Koopmanschap and Rutten
1996; see also Chapter 11).
Does
the difference matter? The
difference in question is that between treating people as carthorses on the one
hand and as sentient flesh-and-blood people (not mere consumers either) on the
other. The issue arises from the fact that humans are both factors of
production and also sentient beings. In some cases public policy emphasizes the
productive role of people, and in others their human characteristics. The tension
in public policy arises from the fact that the best estimate of benefit that
the human capital approach can hope to achieve is a precise measure of the
market productivity of workers. The best to be hoped for from an alternative
based on an evaluation of the consequences for the quality of a persons life,
is a set of relevant and believable measures of characteristics of people and
their working environments features that are not directly marketed at all.
Those characteristics are essentially health and safety. Health services are
marketed, and so are goods and services that contribute to safety, but health
and safety as such are not. They are like the environmental characteristics of
societies that are not marketed even though they have impact on the prices of
assets such as houses (e.g., pollution, noisiness, and beautiful views). They
may not even be marketable, and so cannot be included in the measures of
national accounts.
We
do not go so far as to say that the human capital approach ought never to be
used. However, it should always be accompanied by explicit acknowledgment of
its shortcomings, and used only if the client for the analysis insists upon it
after having considered the alternatives.
The decision-maker approach the safe
passage?
Having successfully negotiated
a passage around both Scylla and Charybdis, we now
turn to our suggested way forward. It may have become clear by now that
underlying the discussion so far is a centrally recurring issue that relates to
objectives, i.e., what are we trying to accomplish, and on whose authority?
Addressing this question occupies the rest of this chapter.
Implicit in the perfect market
approach is the maximand of the total sum of expected utilities. Implicit in
the human capital approach is the maximand of national income, Gross Domestic
Product or Gross National Product. Implicit in many ergonomic studies is the
maximand of worker safety. In others, the criteria are narrowly commercial and
the implicit maximand is profit. Implicit in many health care evaluations is
the maximand of health. A related set of issues concerns matters of equity. How
is fairness or social justice defined, on whose authority, and how ought they
to be embodied in economic evaluations? Addressing each of these issues requires
the exercise of judgment and, in particular, that critically important subset
of judgments generally known as social value judgments. We turn to these now.
Making the unavoidable value judgments explicitly
There are at least three broad
approaches that a reasonable person might adopt in addressing the value
judgments embedded in methods of evaluating workplace interventions. The first
is to adopt an ethical convention commonly employed in a particular discipline,
conventions such as workplace safety or utility maximization. Two
advantages to such a choice are that it has probably been thoroughly worked
over and understood and that one can communicate with fellow disciplinarians on
the basis of an immediately shared understanding of concepts, theories and
their applications. However, this approach has little intrinsic ethical merit,
and some downsides are that the conventions weaknesses may have been glossed
over or largely ignored. Thus, maximizing workplace safety carries the baggage
that it suggests every reduction in workplace hazards as worth undertaking.
Utility maximization carries the baggage that it is only individual welfares of
a particular kind that matter. Moreover, though communication with fellow
disciplinarians may be facilitated, communication with fellow transdisciplinarians may be difficult.
The second approach is to seek
to discover what society thinks are the appropriate value judgments to make. In
pursuing this line, one might trawl public utterances by those with public responsibility,
such as departmental ministers, to discover whether labour market, health, or
employment policy is about maximizing, utility, national income, health or
something else. This is not an easy task, but if accomplished will give an
analysis the moral authority that the previous approach lacked, as well as a
direct communications bridge of understanding. The main reasons why this is not
an easy task is that public utterances of the required sort are few in number,
nearly always ambiguous, at an unsuitably high level of generality, and often
contradictory. Moreover, there are major empirical problems of construct
validity and measurement which remain. There is a further problem: the list of
possible maximands rises as one trawls ministries.
This gives rise to three questions. First, is it sensible somehow to combine
the plurality of objectives in an overall social welfare function? Second, how
are the trade-offs between them to be made? Third, what ought the analyst do about any omitted plausible aims and objectives
that no one claims for their own?
The third approach is to create
a professional scientific consensus, a kind of reference case (Gold et al. 1996), that permits all potential
perspectives, objectives and trade-offs to be taken into account, and that for
any particular study design enables the scope of the analysis, including its
perspective, to be selected according to the values and intentions of the
stakeholders on whose behalf the study is done. The consensus group we have in
mind is the multidisciplinary and multi-professional group of researchers who
investigate the merits of OHS interventions.
This third approach might
involve guessing at what the public utterances would be if they were made less
ambiguously and without contradiction, and adopting them as ones ethical
basis. Alternatively, it might involve seeking a consensus from the ranks of
fellow scientists, or seeking a consensus from amongst those deemed to be
stakeholders. It might be eclectic, seeking to approach evaluative questions in
a flexible way, depending on who were the main clients for the research, or in
multiple ways by evaluating workplace interventions from more than one
perspective, thus exposing important possible differences in the values of
different stakeholders.
We think it is worth trying to
build a professional scientific consensus based on a reasoned attempt to distil
what government, workers, workers families, employers, workers compensation
boards, health and safety regulators, other third party payers, indeed any
stakeholder is seeking to achieve. It can be changed as the distilling becomes
more refined, or as the things distilled themselves change with the changing
political scene. It would be desirable to adopt practical tools derived from it
that are used elsewhere in the same jurisdiction. This may be the best way
forward on the grounds that, done well, the professional approach may come to
be seen as the approach: the one
most persuasive on ethical grounds and, with time, the one most acceptable through
familiarity and clear understanding.
A pragmatist objects
In the health and safety
literature there is a robust tradition of pragmatism, so one may readily
anticipate a pragmatic objection. It runs along the following lines:
theoretical discussion of means and ends, efficiency and equity, science and
ethics, social welfare and the like are rather beside the point. The real point
is that decisions on health and safety are taken on the basis of their impact
on the bottom line. Do they enhance productivity and, if so, do they do so
sufficiently to warrant their undoubted cost to employers? That is all there is
to it. The only question for the analyst is to measure the bottom line effect.
There can be little doubt that this has been the focus of much of the
evaluative literature on workplace health and safety interventions in the past.
More recently, researchers have begun to pay attention to the measurement of
health effects but still largely for instrumental reasons, that is, that they
generate beneficial productivity and hence bottom line consequences. The hope,
of course, is that business managers will be more likely to listen to health
and safety staff, who are all too often at the margins of operational
decision-making, and become allies in the diffusion of interventions for safety
throughout the business.
This is a powerful argument.
Even though it makes fairly heroic assumptions about what it is that motivates
management, it is an argument that scientists ignore at their peril. The
pragmatist is, however, only half right. The bottom line does indeed matter and
the impact of interventions on it needs to be evaluated. But the employers
bottom line is not the only such line and it would seem wise to consider the
balance of advantage over disadvantage from all relevant points of view.
Moreover, in order to know whether the intervention is one worth supporting in
the first place, a broader evaluative framework is implied that takes
everyones interests into account, including the distributional and redistributional consequences.
Two critical levels of analysis
We propose that there are two
critical levels at which evaluative research must operate. One level addresses
the question ought this intervention to be adopted? The second level
addresses the question what is the best way of encouraging the intervention in
question to be adopted?
The first question seeks to
discover what ought to be done. The natural perspective from which to consider
this question entails a social value judgment which we suggest be as
uncontroversial as possible. Therefore, we propose that the perspective from
which this question is addressed be explicit and universal. Our suggestion is
for the perspective also to be the societal one: that is, inclusive of the
health and safety consequences for all possible stakeholders. The advantages of
this approach are several. First, it becomes clear which benefits and costs,
and to whom, are to be included, so that any bias arising out of a less than
comprehensive inventory is exposed and minimized. Second, its starting point is
one in which any cost or benefit can, in principle, be included in the
analysis, making the informational content as complete as possible. Third, for
practical purposes it enumerates an agenda of costs and benefits that can be
further considered by the decision-making clients for inclusion or exclusion
according to their, rather than the analysts, values. Fourth, it enables a
comprehensive view of distributional and redistributional
effects to be taken into account, so that they can be traced, assessed and
their acceptability addressed. Distributional effects are usually important
factors in determining the social desirability of interventions. This inclusive
and universal perspective was also that proposed by the Washington Panel (Gold et al. 1996).
The second question addresses
issues of whose interest it is, or is not, for the intervention to be adopted,
what instruments might be needed in order to persuade those whose interests it
does not match voluntarily to adopt it, or what instruments of regulation and
control might be used that force them involuntarily to adopt it. In most cases
the benefits and costs of greater health and safety will not be distributed
equally across all stakeholder groups. This asymmetry should not to be ignored
by analysts, and empirical research that seeks to assess the significance of
such costs and benefits, whether quantitatively or qualitatively, seems to be
the best way to work out what type of encouragement (e.g., a subsidy or some
form of cost sharing) might be effective in gaining consent in circumstances
where the workplace decision-makers are not convinced of the dominance of
advantage over disadvantage from their own perspective. It seems also to be
wise for researchers to establish the likely size and location of any political
resistance that would arise to regulatory solutions. Here the emphasis is not
on the inherent fairness or unfairness of the consequences of an intervention
but on its acceptability to all affected parties, in order to focus on the
policy implementation issues of persuasion, compensation and enforcement.
A specific proposal and some of its
implications
We seek to define a value-laden
end which can serve as the basis for evaluating OHS interventions, one that is
relatively immune to the criticisms of the perfect market approach, one that
does not treat people as carthorses but is infused with a clear humanity, one
that will enable comparisons to be made across similar activities within the
jurisdiction, such as health care and road safety, so as to avoid significantly
different investment criteria being used, one that preferably uses or adapts
instruments that are widely available and whose characteristics are
well-understood, one that will enable matters of fairness and distributive
equity to be addressed explicitly and analytically, and one that addresses the
informational needs both of workplace parties and of the wider community.
To this end, we propose three
broad framework principles for evaluative analyses. The first ethical
proposition is:
(1) The prime objective of health and safety interventions is to
enhance the expected health-related welfare of individuals in the workplace. It
is not to enhance expected utility or national income.
Supplementary objectives might
include health-related welfare effects on others, such as family members and
care givers, effects described earlier as externalities. The perspective from
which such evaluations ought to take place is thus narrower than the societal
one advocated by many economists (e.g., Gold et al. 1996) but it is different from and broader than the narrow
focus on the business bottom line. It will be necessary to determine the scope
of cost effects that one routinely ought to take account of, as in a reference
case (Gold et al. 1996). This step
also involves making social value judgments. There is a strong case to be made
for flexibility in the choice of perspective, since studies may reasonably take
different views on the grounds that responsibility for managing resources
varies from one situation to another. Common to all evaluations is a focus on
those working in the workplaces and likely to participate in, benefit from or
incur costs as a result of the interventions. Where the emphasis should lie in
any particular study will be a matter for prior determination by researchers
working with research commissioners. The second ethical proposition is:
(2) The perspective of particular evaluative studies will be determined
in conjunction with relevant stakeholders and supplemented where necessary by
analyses that incorporate significant external effects.
The purpose here is to enable a
clear focus on both the pragmatists concern, such as the bottom line, and the
wider interests of other stakeholders. To take an extreme example, a costly
workplace intervention whose benefit falls entirely on workers and their
families in the form of health and which has no productivity impact, may be amply
justified in social terms, but may not be in any individual employers interest
to implement.
The third ethical proposition
concerns equity:
(3) Economic evaluations should, in addition to considering efficiency,
identify potential equity issues of significance in conjunction with
stakeholders and always present results in a way that reveals how the incidence
of costs and benefits falls both immediately and after any predictable market
adjustments have been made.
The distribution of costs and
benefits is important not only so that matters of equity can be addressed, but
also in order to facilitate thinking about how an intervention might best be
implemented. Identifying the incidence of costs and benefits is more difficult
than may appear at first to non-economists in that changing costs of production
will usually generate consequential changes in the type and amount of resources
that businesses will employ, with further consequences for prices and wages
(see Box 5
for definitions). Thus, a cost that may initially appear to be borne by
employers might, as time goes by, come to be passed on to consumers in the form
of higher prices and/or to workers in the form of lower wages. Such effects
will have implications not only for the assessment of the desirability of an
intervention but also for that of its implementation. For example, there seems
little point in compensating employers for cost-increasing measures if the
negative consequences for employers have been passed on to the consumers in the
form of higher prices of their products.
Box 5: The meaning of incidence in economics
What is a little more health and safety
worth?
A little more health and safety
is not of infinite value. If it were, economic evaluation of workplace
interventions to enhance health and safety would be unnecessary. The need for
evaluation arises because the benefits are not infinite, because they are
uncertain, because they come with a price tag and because each of these has an
impact that is different from one stakeholder group to another.
Taking a broad view across an
economy, it seems highly likely that the relationship between the size of
benefit and the number of interventions will be non-linear. A stylized example
is portrayed in Figure 2. In this example we assume that interventions are
ranked from left to right in descending order of their additional contribution
to the benefit. Thus on the far left, machine guards are fitted to those
machines most likely to cause serious injury. As one moves rightward, there lie guards applied to machines that are less likely to
cause a hazardous event and/or have events that are less damaging. On the far
right are guards applied to machines that pose virtually no threat to health
and safety at all. The cumulative benefit always rises as the number of
interventions increases, though it does so at a diminishing rate. At any one
time an economy may be located at particular points on this curve such as a or b, where b represents an economy that has invested more in health and safety
than the economy at a. A more
realistic picture might be that different sectors of an economy are at
different points. So, if we suppose that the manufacturing and the transport
sectors each face the same functional relationship shown in the figure, one
sector may be at point a and the
other at point b.
Figure 2: Conceptualization of the relation
between interventions and consequences
Even if we had sufficient
information to form a judgment about the shape and height of the curve in
Figure 2, this would be insufficient to determine where on the curve one ought
to locate. The flat of the curve is an unlikely segment to choose but there is
plainly much scope for choice in the region to its left. The missing
information is the costs of the interventions, which we may assume not to fall
as interventions increase. Making the simplifying assumption that these are
constant at the level c, the optimal
location is determined at point d.
Additional interventions beyond that point cost more than the amount of benefit
they bring. At points to the left of d
additional interventions add more benefit than they cost. Any such judgment
depends critically on consideration of all the costs and benefits that are
deemed relevant.
Despite its high degree of
simplification, Figure 2 represents the essential character of the solution to
the question what is a little more health and safety worth? The answer
depends on a balancing of cost and benefits, disadvantage and advantage with a
presumption that those projects whose benefits exceed costs ought to be adopted
and those for which that is not true ought not.
The rest of the book will
develop this fundamental model and extend it in various ways, for example, by
including distributional consequences in the evaluation, taking account of risk
and uncertainty, the duration of costs and benefits, and exploring in greater
detail the characteristics that make for high quality research studies of
workplace interventions.
Bibliography
Dorman P (1996). Markets and Mortality.
Cambridge University
Press, New York.
Farr W (1853). The income and property tax. Journal of the Statistical
Society of London,
16, 1-44.
Gegax D, Gerking S, and Schulze W (1991). Perceived
risk and the marginal value of safety. Review of Economics and Statistics, 73, 589-96.
Gold MR,
Siegel JA, Russell LB, and Weinstein MC (1996). Cost-effectiveness in health and medicine.
Oxford University
Press, New York.
Health Canada
(1998). Economic
burden of illness in Canada, 1998. Health Canada,
Ottawa.
Jones-Lee MW (1989). The economics of safety
and physical risk. Basil Blackwell, Oxford.
Jones-Lee MW,
Hammerton M, and Phillips PR (1985). The value
of safety: results of a national sample survey. Economic Journal, 95,
49-92.
Knieser TJ and Leeth
J (1991). Compensating wage differentials for fatal injury risk in Australia, Japan
and the United States.
Journal of Risk and Insurance, 4, 75-90.
Koopmanschap MA, Rutten
FFH, Van Ineveld BM, and Van Roijen
L (1995). The friction
cost method for measuring indirect cost of disease. Journal of Health Economics, 14, 171-89.
Koopmanschap MA and Rutten FFH (1996). A
practical guide for calculating the indirect costs of disease. Pharmacoeconomics, 10, 4606.
Leigh J, Macaskill P, Corvalan C, Kuosma E, and Mandryk J (1996a).
Global burden of disease and injury due to occupational
factors. Geneva:
World Health Organization.
Mill JS
(1965). Principles of political economy with some of
their applications to social philosophy, Book II. In JM Robson, ed. Collected Works of John Stuart Mill, Volume
II. University of Toronto Press, Toronto.
Moore M and Viscusi WK (1988). Workers'
compensation: wage effects, benefit inadequacies, and the value of health
losses. Review of
Economics and Statistics, 69,
249-61.
National
Institute for Clinical Excellence (2004). Guide to the Methods of
Technology Appraisal. London: Institute for
Clinical Excellence.
Petty W
(1691). Verbum Sapienti.
Pritchard C and Sculpher M (2000). Productivity costs: principles and
practice in economic evaluation. London:
Office of Health Economics.
Rees J (1988). Self regulation: an effective alternative to direct
regulation by OSHA? Policy Studies Journal, 16(3), 602-14.
Rosen S (1986). Theory of equalizing differences. In O Ashenfelter
and R Layard, ed. Handbook of Labor Economics, V1, pp. 641-92. North Holland, New York.
Lessons from Health Technology Assessment
Anthony
J. Culyer and Mark Sculpher
Introduction
Economic
evaluation is widely used to assist decision making in health care. The forms
most commonly met are cost-effectiveness analysis (CEA) and cost-utility
analysis (CUA). These methods are well-suited to one of the objectives common
to many health care systems in developed countries, which is to maximise health
subject to a budget constraint. One of the reasons why many societies do not
rely completely on private markets for health care and health insurance is that
markets are imperfect and do not always generate
efficient outcomes. Another reason is that societies may have strong views on
distribution of health and health care, issues that are not easily addressed
through private markets alone.
The
more common market imperfections in health care include the presence of
professional and industrial monopolies, asymmetries of information between
providers and consumers, imperfect agency relationships between health
professionals and patients (and third party payers and health professionals),
supplier-induced demand, externalities, incomplete markets for health care and
health insurance, adverse selection, moral hazard, and the fact that
individuals with limited ability to pay often have the greatest need for care
(for a more complete review of the implications of these factors, see Culyer
1991).
While the markets for many goods and services are characterized by the presence
of some of these features, few are so thoroughly imbued with all of them. The
workplace health and safety field has many of these same characteristics as
health care (see the discussion in Chapter 2 for details) and, in addition, is
markedly affected by the ways in which the labour market operates, which is
beset by further market failures.
In
light of the weaknesses of much of the economic evaluation work that has been
conducted to date in workplace health and safety (see Chapter 3 for details),
there is good reason to consider the lessons that can be learned from health
technology assessment, where methodologies and the use of economic evaluation
in policy decision making are much more advanced. Hence, in this chapter we
draw on the experiences in health technology assessment to inform the use of
economic evaluation in occupational health and safety (OHS), and touch on some
of the problems that arise in connection with the application of these methods
in health and safety interventions, especially those that differentiate their
application in this field from applications in health care. We also provide a
checklist to help researchers to design better studies, and to help researchers
and research consumers alike to assess the quality of studies better than has
usually been the case. Finally, we discuss the arguments for developing a
reference case.
Economic evaluation in the policy context
Policy context in health care
As
has just been noted, economic evaluation has been used widely in the health
care sector as a key element in funding and formulary decisions, clinical guideline
development and other health policy planning. However, establishing the
cost-effectiveness (or its absence) of various interventions in the health care
setting is a costly undertaking and in general is prohibitively expensive for
individual hospitals, small health regions or even provinces like those found
in Canada. For this reason, high-level arms-length bodies have emerged such as
the National Institute for Health and Clinical Excellence (NICE) in England and
Wales, the Pharmaceutical Benefits Advisory Committee in Australia and the
Common Drug Review process in Canada, which provide evidence on the economic
merits of health technologies and which are intended to inform national
decision making. These organizations review existing evidence related to the
costs and consequences of health care interventions and employ standard
evaluation techniques in order to make recommendations to regulators, drug
plans, health regions or governments (regional and national). Likewise, in a
workplace health and safety context, there may be interventions of relevance to
many industries, firms, and workers, but it will often be too costly for
individual firms to evaluate them and the benefits of doing so will flow well
beyond the confines of any individual organization. This suggests that health
and safety evaluation studies have some of the characteristics of a public good
and that those which are undertaken will often be of use to a number of
organizations, particularly if such studies were to present results in a way
that facilitated both a comparison with other evaluations and an assessment of
generalizability of the results.
A dual purpose in the evaluation of
workplace interventions
In
health care, economic analyses typically take a single perspective (such as that
of the payer or health care system as a whole), whereas in other contexts there
is value in studies considering costs and consequences from a range of
different perspectives such as those of employers, workers, workers families,
injured workers care-givers, insurers, and public authorities. This is likely
to be the case in evaluating workplace interventions.
Considering
multiple perspectives highlights two possible information roles for economic
evaluation. First, it serves to identify those interventions that are worth
undertaking from whichever perspective is selected. This purpose is, therefore,
that of helping decision makers to form a view as to whether, on balance, an
intervention ought to be adopted. Second, evaluations can help to identify the
reasons why some apparently worthwhile interventions are not adopted by
highlighting the way in which the gains and losses from implementation are
distributed across different groups. For example, a workplace intervention
whose benefits accrue mainly to workers but whose costs fall mainly upon
employers is less likely to be implemented, even if overall benefits exceed
overall costs, than one in which the benefits and costs are both realized
entirely by employers. Not all evaluations of interventions will meet the
criteria of a full-scale social welfare maximization exercise, since the
informational requirements of such an analysis are substantial. But they can
still provide information to workers and employers that can be used in the
bargaining process, thereby reducing asymmetries of information, and they can
increase the information available to higher-level decision makers seeking to
form an overall judgment of the worthwhileness of inventions of various kinds.
We
shall assume that both information roles are equally as important. The first
helps to establish the social worthwhileness of interventions (and their
appropriate scale), and the second helps to identify the steps that might need
to be taken in order to ensure implementation, either voluntarily, through
regulation, or through subsidy. In addition, the second role can help identify
specific distributional matters that ought to form part of the assessment of
social worthwhileness seen through the lens of equity or social justice.
The methods of economic evaluation
The National Institute for
Health and Clinical Excellence (NICE) in the UK, more than any other health care
agency, has made the use of economic evaluation a key decision tool for public
policy regarding the introduction and manner of use of health care
technologies. Given the parallels between the challenges faced in the health
care sector and those in OHS, there is clearly value in examining the ways in
which agencies such as NICE have employed standardized economic evaluation
techniques to inform the resource planning process across diverse groups
(patients, care providers, insurers). We draw on their experience in the rest
of this chapter.
Different types of analysis
There are
broadly four kinds of economic evaluation, each of which can be found in the
literature of health economics: cost-benefit analysis (CBA) (sometimes called
benefit-cost analysis), CEA (sometimes called cost-efficiency analysis), CUA,
and cost-minimization analysis (CMA). In addition, cost-consequence analysis
(CCA) compares disaggregated costs and consequences of options without
attempting to add or combine them in any way, leaving these tasks to the
decision maker (see Box
1 for summary descriptions and Chapter 9 for details). Although
cost-consequence analysis has generally been thought to fall short of a full
economic evaluation in health care, it is often a useful precursor to a
full-fledged analysis and it is a helpful framework for dealing with multiple
perspectives. For the purpose of our discussion here, it suffices to say that
the primary difference between the various types of economic analyses is the
metric used for the key consequences (the terms benefit, outcome, and
effect are also used regularly in place of consequence).
Box 1: Types of economic evaluations
Although there
are important differences between the different types of economic evaluation
(see Sculpher et al. 2005), they have shared
features. Each requires the calculation of present values of cost and benefit
using a social discount rate. Each requires the systematic comparison of all
the relevant effects of proposed alternative interventions with a view to
determining: (1) which intervention, scales of intervention, or combination of
interventions, produces the best outcome (either minimum cost or maximum
difference between benefits and costs) or (2) the magnitude of the benefit that
can result from interventions having similar costs. Depending on the
perspective of the analysis, costs falling on different affected parties (e.g.,
health system, patients) will be included. Each customarily uses sensitivity
analysis for assessing the robustness of the conclusions in the face of
variations in the assumptions and uncertainty in the evidence used. Other
common characteristics are explicitness in the objectives, assumptions and
methods, and consistency in the principles guiding the choice among alternatives.
Opportunity cost
Each type of economic
evaluation relies on the concept of opportunity cost. Opportunity
cost is the value of a resource in its most highly valued alternative use. In a
world of perfect markets in which all goods are traded, opportunity costs are
revealed by the market prices of resources, since these prices represent the
lowest sum of money required to bid the resources away from their most highly
valued possible alternative uses. Where the stringent conditions required for
perfect markets are not met, opportunity costs and market prices can diverge
and true opportunity costs (shadow prices) may need to be imputed. The
opportunity cost of a resource already owned by an organization is not usually
revealed through a market price. The best alternative may be an alternative use
within the organization but it is not revealed by competitive bidding between
managers but through planning processes, with the opportunity cost being
elicited through discussion and judgment, without the cost necessarily being
cast in terms of money.
One example of the
importance of opportunity costs arises in health technology assessment when a
budget-constrained health care system is considering funding a new technology
which will impose additional costs. To balance the budget an existing
technology/program will have to be removed. The aim of economic evaluation
methods is to assess whether the benefits of the new technology outweigh the
opportunity costs.
Opportunity costs should
not be confused with transfer payments. When trades take place in a monetized
economy, payments reflect the compensation required for resource owners to part
with something of value. Transfer payments, on the other hand, are not made in
exchange for resources and so do not measure the value of any such resources.
They are merely a transfer of purchasing power from one individual or group to
another. Box 2
identifies alternative concepts of costs and prices. Chapter 10 elaborates on
these constructs. In general, opportunity cost cannot be defined independently
of the decision-making context, since it involves identifying the expected
consequences of alternative courses of action, and so cannot simply be read off
conventional financial accounts.
Box 2:
Alternative concepts of costs and prices
Analytic
perspective
Analytic perspective refers to the nature of the analysts role and
task in the context of an economic evaluation. One common perspective is often
termed the social decision-making perspective. Under the social
decision-making perspective, the analyst addresses questions of concern to, and
the values of, the decision maker or the organization in which (s)he operates. In one form of this, the analyst plays
the role of consultant, having the social decision maker as client. In another,
the organisation has its objectives and
constraints explicitly defined, for example by a higher policy making body, and
these can guide the analyst. Another analytic perspective is termed the
societal perspective. This usually entails the analyst defining a more or less
broad concept of social welfare and making explicit the social value judgments
involved in so doing. With this approach there is the risk that the analyst
adopts criteria that are seen as irrelevant by real world decision makers.
Other perspectives are more particular, for example those of the owners of
businesses, or (not the same thing) the managers of businesses, or unionized
workers, or all workers, or workers families, or third party payers (such as
workers compensation boards). The things that count as benefits and costs,
and that get caught up in externalities, can vary
significantly depending on which viewpoint is adopted. A major guiding
principle of all economic evaluations is consequently that the analytic
perspective must be stated explicitly so that readers can assess for themselves
the consequences by way of inclusion or exclusion of the various possible
effects for the decisions informed by the analysis.
Value
judgments
All forms of
economic evaluation require value judgments. The choice of perspective itself
commits the analyst to particular value judgments. In addition, the analyst
needs to make other critical choices, all of which involve value judgments,
some of which may be more specific and precise than the ones directly or
indirectly implied by the values embodied in the chosen perspective. For
example, a perspective emphasizing health may specifically entail selecting the
QALY as an outcome; a perspective emphasizing social cost may specifically
select costs falling on the public sector; and a general requirement for equity
may need specific decisions relating to the weighting of consequences based on
whether a dollar is gained/lost by stockholders or
workers. A decision to treat monetary consequences with equal weights
regardless of who is experiencing the loss or gain is not a means of escaping
the value issue. On the contrary, it is to make a very specific value judgment,
which is that it is appropriate to value each dollar of consequence equally.
Evaluation of interventions the health technology
assessment experience
In
the health care field the word technology is used quite broadly to refer to
a means of accomplishing something. It includes the use of health care
technologies such as scanners, prescription drugs, bed rest, and watchful waiting.
Although less frequently encountered there, it applies also to the evaluation
of technologies of governance and managerial arrangement. Counterparts in OHS
might be the use of machine guards or ergonomically designed workstations and
the use of OHS management systems.
Health
technology assessment (HTA) has had an increasingly prominent position in
health care policy internationally. Although much HTA research has been funded
and published since the late 1960s, it was not until the mid-1990s that it gained
a formal foothold in policy making.
In the last decade, many health care systems in developed countries have
decided to inform decisions about the adoption of new health interventions by
use of economic evaluation of the clinical and epidemiological evidence. While
these requirements have been applied principally to pharmaceuticals, the range
of technologies requiring such evidence before adoption has tended to be
broadened over time (for example, public health interventions were added to
NICEs range of responsibilities in 2005). A formal requirement for economic
analysis to support reimbursement or coverage began in the public systems of
Ontario, Canada (Ministry
of Health 1994)
and Australia (Commonwealth Department
of Health 1992),
but have since spread widely (Hjelmgren et al.
2001).
Australia, Belgium, Canada, England and Wales, Israel and Scotland have all
published guidelines for economic evaluations as inputs into decisions about
coverage and reimbursement (Tarn
and Smith 2005).
The
methodology of economic evaluation has developed rapidly over the last 40
years. The research methods used for health care system decision making today
are much more sophisticated than those employed in the past. Early economic
evaluations commonly assumed (often only implicitly) that the objective of
health care was to maximise gross domestic product. This may be illustrated by
an analysis of the economic consequences of preventing the birth of babies with
Downs Syndrome through screening (Hagard and Carter 1976). In this study the benefits
of screening were seen in terms of avoiding the costs of caring for and
educating a child with Downs Syndrome, implicitly assuming that there was no
intrinsic or even human capital benefit to a life (Culyer
1987).
As noted in Chapter 2, the naive human capital approach to valuing the benefits
of health care fails to recognise that individuals value health for reasons
other than the productive potential it generates and they value lives for
reasons other than the gross domestic product each life may manufacture (net,
of course, of human maintenance costs) (Mishan 1971; Blades et al. 1987).
For
much of the subsequent period it became increasingly clear that there were
serious tensions between the principles of standard welfare economics
(essentially the societal perspective described above) and a more flexible and
decision-oriented perspective on evaluative research towards which many health
economists were leaning. Though standard welfare economics gives clear guidance
on what is meant by efficiency, how costs and benefits should be measured, what
perspective should be taken, and whether the adoption of a new health technology
improves social welfare, it has strong normative underpinnings which require
leaps of faith to accept (Sculpher et al. 2005).
Essentially,
welfare economics has a number of significant and controversial implications
for evaluation in health care. The first is that heath care programs should be
evaluated in the same way as other programs. The concern here is that standard
welfare economics relies on a particular construct of efficiency known as a
potential Pareto improvement measured by a compensation test like can the
gainers compensate the losers either in theory or practice and still retain
a net gain? The criteria are meant to ensure that there are no utility losses
after suitable compensation, only utility gains, since the principles of
welfare economics do not allow one to make a direct comparison of the value of
utility losses to one individual with the value of gains to another (see Box 3 for more
detailed definitions). An outcome where there are some utility gainers and no
net utility losers is considered to mark an unambiguous gain in social welfare.
The
standard welfare economics approach is not well-suited to addressing matters
such as whether an intervention improves life expectancy or health, which is
the standard clinicians or health policy decision makers question. It focuses
on the much more obscure matter (from clinicians or policy makers viewpoint)
of whether the intervention improves utility. The clinicians or health policy
decision makers approach is, however, the basis of outcome metrics known as
health-related quality of life (HRQL) measures and many health economists
essentially adopt an approach that is based on the idea that health services
exist primarily to create health rather than utility.
Box 3: Pareto constructs
A
second controversial aspect of welfare economics is an implicit view that the
current distribution of income is, if not optimal, then at least acceptable (Pauly
1995)
and that the distributive impact of a decision based on economic evaluation is,
or ought to be, negligible. Other controversies include the conditions of
rationality and consistency that are required for individuals to maximise their
utility, which have been shown to be violated in most choice situations (Machina 1987), and the problem of second best (e.g., Ng
1983),
whereby first best solutions in a second best world (i.e., a situation where
only some of the conditions of the ideal solution are met) may actually
represent a reduction in social welfare as defined by the potential Pareto
criterion.
There
is an alternative to the standard welfare economics approach to economic
evaluation in health care. In the United Kingdom and elsewhere, an approach
described as extra welfarist (Culyer
1991) has provided the
methodological foundations of economic evaluation in health care (see Box 4 for
details). It is a version of the social decision-making perspective and uses
cost-utility analysis rather than CBA. It is based on an exogenously defined
objective (such as population health maximization) and an exogenously
determined budget constraint for health care. The efficiency problem is thereby
transformed into another constrained maximization problem (i.e., how to
maximize the amount of incremental health produced by a given budget). This
pragmatic approach is well-suited to partial analyses that assume that there
are few significant repercussions of health care decisions beyond the health
sector itself. Correspondingly, it is not well-suited to the analysis of inter-sectoral choices, where the outcome measures will typically
be different and pose major issues of relative valuation, and where opportunity
costs may become difficult to identify.
Box 4: Welfarism and extra-welfarism
One
of the implications of using the extra-welfarist approach in health care is
that it facilitates a multi-disciplinary outlook to the research, requiring the
identification and synthesising of relevant clinical and other evidence;
mathematical models to characterise the natural history of a given disease and
the effects of interventions; the definition of measurement and valuation of
health gain; and quantification and valuation of the resource implications.
Hence, major contributions to this research are made by various disciplines
including clinical science, cognitive psychology, decision science,
epidemiology, medical statistics, and operations research, in addition to
economics.
Differences
in the sources and treatment of bias
A
major difference between the information available for an economic appraisal in
health care compared to that available for workplace intervention evaluation is
the character and treatment of bias. In evaluating the effectiveness of medical
technologies (in particular drugs), randomisation is often used in clinical
trials to control for potential confounding factors, whereas this is rarely
possible in workplace intervention evaluation. Both the location and the size
of workplace evaluations rarely permit randomization. Thus, it becomes
necessary to anticipate confounders as best as may be possiblefor example by
measuring them explicitly in observational studies for subsequent multivariate
analysis or, minimally, by exercising well-informed judgment. The careful use
of sensitivity analysis often enables the identification of omitted variables
or poorly measured ones, as well as giving an indication of the extent to which
the changes in outcome attributed to the intervention are robust.
A
second source of bias relates to the decisions made by the analyst about the
costs and consequences that are to be measured, how one is traded off against
another, and how to add them up across different individuals (see Chapter 2 for
a more detailed discussion of these issues). These matters may be of less
concern in health care because costs and consequences are less often
distributed across such varied categories of stakeholders. In general, there is
no right answer to these questions. The answers are likely to be controversial
and raise major questions of policy, politics, ethics and public acceptability.
This is not an argument for helplessness, for the identification of such issues
is an important part of the decision making process and any measurement of
relevant dimensions will usually be helpful. The conclusion therefore is that
analysts ought to be open and explicit about the value content of their
analyses, to face up directly to the challenges that rival values might pose, and
whenever useful, to subject value judgments to the same kind of sensitivity
analysis that is recommended for design attributes. The merit of this approach
is in identifying value judgments that do or do not, as the case may be, affect
the major results of the analysis, and providing decision makers with such
evidence about values that may have a bearing on their decisions.
A brief description of current key
methodological guidance
As
economic evaluation has become more widely undertaken and formally used in
health care decision making, much energy has gone into developing
methodological guidelines for researchers. In general, these can be divided
into two categories: guidelines developed as a scientific statement of good
practice in the field, and guidelines issued by particular decision-making agencies to define the approach to economic
evaluation deemed to be appropriate in their jurisdiction.
With
regard to scientific statements of good practice, two particularly
authoritative documents are worth noting. The first is a widely known textbook,
Methods for the Evaluation of Health Care Programmes, now in its third
edition (Drummond et al. 2005). A consistently important
element of this book since its first edition has been its inclusion of a
methods checklist for critiquing economic evaluation studies. An adaptation of
this is reproduced in Table 1. Essentially, the checklist focuses on the need
for clear description of a study and the use of those methods that are
considered to be good practice in economic evaluation. The list emphasises key
aspects of a sound evaluation such as explicitly stating the perspective used
in the analysis, using incremental analysis, discounting future costs and
consequences, and giving adequate attention to uncertainty in the estimates and
to the implications of omitted relevant variables. The need for such a list
became clear from reviews of earlier evaluations, most of which were deficient
in many more than just one or two respects.
<insert Table 1, found at end of document, about here>
The
second document was developed by a multi-disciplinary panel convened by the US
Public Health Service and published in 1996 (Gold et al. 1996). It too provides a
description of methods issues and recommendations for good practice. This text
is more prescriptive in its recommendations than Drummond et al. (2005). It also introduced the idea
of a reference case, a concept to which we return later. Key aspects of the US
Panels recommendations were:
·
A societal perspective should be taken.
In part, this relates to resource costs, and requires that costs falling both
on a health care budget and outside it should be included in analyses.
Importantly, it requires inclusion of costs such as travel costs borne by
patients and time costs borne by relatives caring for patients. The US Panel
took an innovative view on the treatment of the productivity effects of health
interventions. They concluded that, in part, these would already be captured by
the valuation of health (they recommended use of the QALY as the outcome
measure), while residual productivity effects (such as those falling on the
wider community through, for example, reduced taxation) ought to be explicitly
included. The choice of a societal perspective also implies the inclusion of
all health and non-health effects (both positive and negative) to intended
recipients and others. Evaluative studies of workplace interventions have
typically left the issue of perspective implicit. Some appear largely to view
evaluation through a workers lens and other through an employers lens.
Virtually none has systematically taken a more comprehensive view.
·
Health effects should be expressed in terms
of QALYs. This is a measure of health which incorporates the effects of
interventions on both mortality (through changes in survival duration) and
morbidity (through effects on health-related quality of life). The U.S. Panel
thus embraced CUA/CEA as the appropriate analytic paradigm. In the workplace
intervention evaluation literature there is no convention regarding the
measurement (or even the relevance) of health effects, other than through its
impact on productivity.
·
Effectiveness estimates from best-designed and
least-biased sources should be used. Reflecting the typical limitations and
heterogeneity of the clinical evidence base available for economic evaluation,
this recommendation leans towards using best available evidence. The point can
also apply to sources of non-clinical evidence such as resource costs. Other
guidelines have emphasised the importance of incorporating all evidence given
the hazards of selecting best evidence (National Institute for
Clinical Excellence 2004).
As noted earlier, effectiveness evidence is more likely to be biased in various
ways when based on data observed in workplaces. Assessment of bias or the
quality and generalizability of evidence is rarely addressed in any systematic
way in workplace intervention evaluations.
·
Comparison should be made with existing
practice and (if necessary) viable low-cost alternatives. Comparator
technologies (minimally the status quo) are always necessary. However,
decisions about the range of options to compare within an economic evaluation
are central to the appropriate specification of an economic evaluation to guide
decision-making. Leaving out a relevant option can result in highly misleading
results. Comparators are rarely used in workplace evaluations and, where they
are, they are rarely described explicitly.
·
One-way and multi-way sensitivity analysis
(for important parameters) should be undertaken. It is recognised that all
analyses will be characterised by uncertainty about key elements of evidence.
Sensitivity analysis is, as has been seen, a means of exploring the extent to
which the conclusions of a study are robust to the changes in the value of key
inputs. In analysing workplace interventions, problems of incompatible values
and political differences are likely to loom more prominently than in the case
of the clinical literature, so sensitivity analysis ought also to be used to
test the dependence of the conclusions on controversial value judgments.
Sensitivity analysis is virtually unknown in the evaluative literature of
workplace interventions.
There are now many methods guidelines
issued by decision making agencies.
These have recently been surveyed by the International Society for Pharmacoeconomics and Outcomes Research (Tarn
and Smith 2005).
They display considerable variation, both in terms of how prescriptive they are
and in their specific recommendations. Table 2 illustrates the variation using
the example of recommendations for the selection of options for comparison.
Table
2: Variation in recommendations for comparator technologies reproduced from Sculpher
and Drummond (2006)
based on data from Tarn and Smith (2005).

The National Institute for Health and
Clinical Excellence (NICE) in the UK issued methods guidelines for analyses
being undertaken as inputs to its Technology Appraisal Programme (National Institute for
Clinical Excellence 2004).
The guidelines set out the requirements for economic evaluation based on the
characteristics of the decisions that the organization is charged to make and
the specific constraints under which it operates. NICEs recommendations are
prescriptive and go beyond those of the US Panel in a number of respects.
Notable recommendations are:
·
The use of systematic reviews to identify all
appropriate evidence on effectiveness for economic evaluation.
·
The use of a validated generic measure of
health-related quality of life as a basis for formulating the morbidity
component of QALYs.
·
Restrictions on the types of costs and
consequences to a set deemed relevant by policy makers in the Department of
Health (the perspective taken is essentially that of public sector managers).
·
The use of probabilistic sensitivity analysis
which, simultaneously, assesses the implications of uncertainty in all
parameters within an evaluation and allows this to be presented in terms of the
probability that a particular option is the most cost-effective, conditional on
how much the health care system is willing to pay for a QALY (Claxton et al. 2005).
Case for a reference case
A
key feature of both the US Panels statement of good practice in economic
evaluation and NICEs 2004 methodological guidance is the definition of a
reference case. The purpose of a reference case is to provide consistency in
methods used in all evaluations regardless of the disease areas or technologies
being evaluated.
The
need for consistency is a response to two important features of economic
evaluation in health care. The first is the lack of consensus about some areas
of methodology. These include the choice of study type (e.g., CUA vs. CBA), the
source of preference and value data (e.g., patients versus the general public),
the approach to describing health states for valuation, and the inclusion of
future costs that appear to be unrelated to the intervention of interest but
are incurred because life expectancy is extended by the intervention. By taking
a position on each of these, a reference case can be seen as either defining an
authoritative view about the most appropriate method, or as simply selecting
one approach in order to avoid unhelpful variability between analyses. The
second feature of consistency between studies relates to pragmatic uncertainty.
This relates to the need for decision makers to specify their preferred
methods, in particular as they embody political or value content in the policy
context in which the analysis is to be used. For example, they may wish to be
explicit about what they consider to be the appropriate cost perspective and
the types of equity issue to be considered.
Stipulating
a reference case does not preclude analysts undertaking other types of analysis
(e.g., different approaches to health valuation). However, such alternative
approaches would need to be undertaken in addition to the reference case and should be justified on
the basis of potential shortcomings of the reference case in a specific
context.
Would
a reference case be helpful to guide researchers undertaking economic evaluations
in the context of OHS interventions? It is clear that there is even greater
lack of consensus about appropriate evaluation methods for workplace
interventions than in health care (see Chapter 3). As a result, the vast
majority of studies do not meet the minimal quality requirements in the
checklist and it is virtually impossible to make comparisons between the
effectiveness, let alone the cost-effectiveness, of alternative interventions
reported in different studies. There is, however, an important
difference between work-related interventions and health care: there is no
single decision maker (such as a reimbursement agency in health care) for whom
the analysis is undertaken, and who might be perceived as having an
authoritative set of objectives and constraints that ought to be reflected in
the methods chosen for the economic analysis. Rather, policy changes relating
to workplace health and safety are more likely to be based on interactions
between key stakeholders. These include employers (who are likely to incur much
of the cost of interventions and only a portion of benefit in terms of
productivity changes), as well as labour representatives, workers compensation
and insurance boards, government and regulators. Therefore, any reference case
in this area would need to reflect the multiple perspectives that may be had in
any particular decision context. It would be appropriate for the reference case
to stipulate a societal perspective on costs, health effects and other effects
which would indicate what should be done considering the net cost and effects
on everyone. However, it would also be necessary for the reference case to
require that analyses include estimates of the distribution of costs and effects between stakeholders, which
would provide both the various parties affected with a basis for policy
negotiations and political decision makers with a basis for making an overall
assessment.
Conclusions
The
way in which the labour market determines decisions about health and safety is fraught
with imperfections. This suggests that a reliance on market mechanisms alone is
unlikely to deliver the optimal degree of prevention, protection or
compensation. The labour market is also the classic setting for political
conflict between labour and employers. It can generate profound inequalities in
society which many may regard as inherently and deeply unjust. For such
reasons, if economic analysis is to be used to replace or substitute for the
market mechanism it needs to offer a methodology that does not replicate these
imperfections, nor one that introduces new and no less unsatisfactory biases.
One way may be to simulate the operation of a perfect market (this is, in
essence, the objective of economic evaluations done according to the customary
rules of neoclassical welfare economics) and the other is to postulate specific
objectives and constraints that are appropriate to the sector and problem at
hand (this is, in essence, one manifestation of the social decision-making
perspective).
We
do not advocate either in preference to the other here. However, what we do
suggest is that analysts ought to be as explicit as possible about the key
structural elements of their analyses, their sources of evidence and the values
embodied in their interpretations of findings. We have provided a checklist
based upon one commonly used in health technology assessment. It serves to
assist those wishing to undertake well-designed workplace intervention studies
with economic components, and those wishing to compare or evaluate existing
studies.
Bibliography
Blades CA,
Culyer AJ, and Walker A (1987). Health service efficiency: appraising
the appraisers - a critical review of economic appraisal in practice. Social Science & Medicine, 25, 461-72.
Claxton K, Sculpher M, McCabe C, et al. (2005). Probabilistic
sensitivity analysis for NICE technology assessment: not an optional extra. Health Economics, 14, 339-47.
Commonwealth
Department of Health, Housing and Community Services (1992). Guidelines
for the pharmaceutical industry on preparation of submissions to the
Pharmaceutical Benefits Advisory Committee. Canberra: AGPS.
Culyer AJ (1987). The scope and limits of health economics (with reference to
economic appraisals of health services). In Oekonomie des Gesundheitswesen, Jahrestagung des Vereins für
Socialpolitik, Gesellschaft für Wirtschafts- und Sozialwissenschaften, Neue
Folge Band, 159, pp. 31-53. Duncker &
Humblot, Berlin.
Culyer AJ (1991). The normative
economics of health care finance and provision. In A McGuire, P Fenn, and K
Mayhew, ed. Providing health care: The
economics of alternative systems of finance and delivery, pp. 65-98. Oxford University
Press, Oxford.
Drummond M,
Sculpher M, Torrance GW, O'Brien BJ, and Stoddart GL
(2005). Methods for the economic evaluation of health care
programmes. Oxford University Press, Oxford, UK.
Gold MR, Siegel JA, Russell LB, and Weinstein MC (1996). Cost-effectiveness in health and medicine. Oxford University
Press, New York.
Hagard S and Carter FA (1976).
Preventing the birth of infants with Down's syndrome: a
cost-benefit analysis. British Medical Journal,
1, 753-56.
Hjelmgren J, Berggren F, and Andersson F (2001). Health
economic guidelines--similarities, differences and some implications. Value Health, 4, 225-50.
Machina
MJ (1987). Choice under uncertainty: problems solved and unsolved. Journal of Economic Perspectives, 1, 121-54.
Ministry of
Health (1994). Ontario
guidelines for economic analysis of pharmaceutical products. Toronto, ON:
Ministry of Health.
Mishan EJ (1971). Evaluation
of life and limb: a theoretical approach. Journal of Political Economy, 79,
687-705.
National
Institute for Clinical Excellence (2004). Guide to the methods of
technology appraisal. London:
National Institute for Clinical Excellence.
Ng YK
(1983). Welfare economics: introduction and development of basic concepts. Macmillan,
London.
Pauly MV
(1995). Valuing health care benefits in money terms. In FA Sloan, ed. Valuing
health care. Costs, benefits and effectiveness of pharmaceuticals and other
medical technologies, pp. 99-124. Cambridge
University Press, Cambridge.
Sculpher M
and Drummond M (2006). Analysis sans frontières:
can we ever make economic evaluations generalisable
across jurisdictions? Pharmacoeconomics,
24, 1087-99.
Sculpher M,
Claxton K, and Akehurst R (2005). It's just
evaluation for decision making: recent developments in, and challenges for,
cost-effectiveness research. In PC Smith, L Ginnelly, and M Sculpher, ed. Health policy and
economics. Opportunities and challenges, pp. 8-41. Open
University Press, Maidenhead.
Tarn TY and Smith MD (2005).
Pharmacoeconomic guidelines around the world. ISPOR
Connections, 10, 5.
Table 1. A checklist for assessing economic
evaluations based on Drummond
et al. (2005).
|
1. Was a well-defined question posed in answerable form?
1.1 Did the study examine
both costs and effects of the intervention?
1.2 Did the study involve
a comparison of alternatives?
1.3 Was a perspective for
the analysis stated and was the study placed in any particular decision-making context?
2. Was an adequately
comprehensive description of the competing alternatives given? (i.e., can you
tell who did what to whom, where, and how often for each option?)
2.1 Were all relevant
alternatives included?
2.2 Was a do-nothing
alternative considered? If not, were there good reasons why it was
inappropriate?
3. Was the
effectiveness or ineffectiveness of the intervention established?
3.1 Was this done through a randomised,
controlled trial? If so, did
the trial protocol reflect what would happen in regular practice?
If not, how were confounding factors controlled?
3.2 Were effectiveness data collected and
summarised through a
systematic
review of studies? If so, were the search strategy and rules for inclusion or
exclusion outlined?
3.3 Were observational
data or assumptions used to establish effectiveness? If so, what were the potential
biases in the results?
3.4 If the study was an efficacy study, was any attempt made to
assess its generalisability?
4. Were all the
important and relevant costs and consequences for each alternative
identified?
4.1 Was the range wide
enough for the research question at hand?
4.2 Did the range include
material useful to all relevant perspectives?
4.3 Were all relevant
costs (labour, capital, as well as operating costs) included?
4.4 Were all relevant
consequences (for all parties potentially affected, whether or not engaged in
the workplace) included?
5. Were
costs and consequences measured accurately in appropriate physical units
(e.g., hours of nursing time, number of physician visits, work days gained or
lost, life-years gained or lost, effects on workers families)?
5.1 Were
the sources of resource utilisation described and justified?
5.2 Were any possibly
significant costs or consequences omitted from consideration or, if
identified, not measured well? What weight did they carry in the subsequent
analysis?
5.3 Were there any
special circumstances (e.g., joint use of resources) that made measurement
difficult? Were these issues handled appropriately rather than being simply
ignored?
6. Were costs and
consequences valued credibly?
6.1 Were the sources of all values clearly
identified? (Possible sources include market values, worker or employer
preferences and views through surveys, policy makers' views and health
professionals' judgments.)
6.2 Where market values
were absent (e.g., value of family care-givers time) or did not reflect
actual values (such as clinic space donated at a reduced rate), were
adjustments made to approximate market values?
6.3 Was the valuation of consequences
appropriate for the question posed (i.e., was the appropriate type of
analysis (CEA, CUA, CBA) selected)?
7. Were costs and
consequences adjusted for differential timing?
7.1 Were costs and
consequences occurring in the future discounted to their present values?
7.2 Was any justification
given for the discount rate(s) used?
8. Was an
incremental analysis of costs and consequences of alternatives performed?
8.1 Were the additional
(incremental) costs generated by one alternative over another compared with
the additional effects, benefits, or utilities generated?
9. Was allowance
made for uncertainty in the estimation of costs and consequences?
9.1 If workplace level
data on costs or consequences were available, were appropriate statistical
analyses performed?
9.2 If a sensitivity
analysis was employed, was justification provided for the ranges or
distributions of values (for key study parameters), and the form of
sensitivity analysis used?
9.3 Were the authors
conclusions sensitive to the uncertainty in the results, as quantified by the
statistical and/or sensitivity analysis?
10. Did the
presentation and discussion of study results include all issues of concern to
users?
10.1 Were the conclusions
of the analysis based on some overall index or ratio of costs to consequences
(e.g., cost-effectiveness ratio)? If so, was the index interpreted
intelligently or in a mechanistic fashion? If not, was any guidance offered
as to how decision makers might seek to make an overall judgment of
effectiveness or cost-effectiveness?
10.2 Were the results compared
with those of others who have investigated the same or similar question? If
so, were allowances made for potential differences in study methodology?
10.3 Did the study discuss
the generalisability of the results to other settings, workplaces or industrial
sectors?
10.4 Did the study allude
to, or take account of, other important factors in the choice or decision
under consideration (e.g., distribution of costs and consequences, political
constraints, or relevant ethical issues)?
10.5 Did the study discuss
issues of implementation, such as the feasibility of adopting the preferred
program given existing financial or other constraints, and whether any freed
resources could be redeployed to other worthwhile programs?
10.6 Did the study involve key stakeholders at relevant phases, such
as the choice of intervention and comparators, selection of research
question, selection of workplaces, choice of value judgments (such as the
weights to be attached to dissimilar consequences), the concept of equity to be
used, and the ease of implementation in the short, medium and long term?
|
 Return
to index
Return
to index
Journal of Health Economics
The Journal of Health Economics welcomes
articles on the economics of health and medical care written for a readership of health economists. Karl
Claxton, Andy
Street, Luigi Siciliani
and I are the editors with responsibility for all non-US
articles. The address to which submissions should be sent is on the
Elsevier website: http://ees.elsevier.com/jhe/.
Enquiries by e-mail may
be made to me on ajc17@york.ac.uk or
Karl on kpc1@york.ac.uk or Andy on ads6@york.ac.uk or Luigi on ls24@york.ac.uk
or to the Journal
secretary, Michelle Hickman on journal-health-econ@york.ac.uk
 Return
to index
Return
to index
Anglican chants
ANGLICAN
CHANTS FOR PSALMS
These chants
have each been written with a specific psalm in mind. I have tried to capture
the feel, especially of the opening verses. Of course some psalms have many
moods and these cannot always be accommodated simply by varying the way the
psalm is sung (harmony or unison, lower or upper voices, full or semi-chorus, cantoris or decani, with or
without cantor, solo with hummed accompaniment, with or without antiphons,
etc.). The only recourse then is to another chant and then possibly yet
another. I have provided for this in the most obvious places. Moods that are commonly not embraced by the
music include pain, anguish and despair. I have tried to remedy this.
I have tried
to match the structures of the chants to those of the psalms: synonymous,
antithetical, constructive, climactic, but especially to the groupings of the
verses, and not only through the obvious means of single, double, triple and
quadruple chants.
Tony Culyer
Toronto 2012
SINGLE
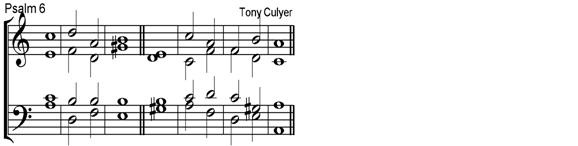
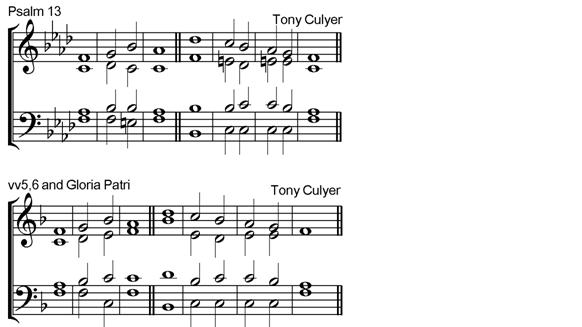
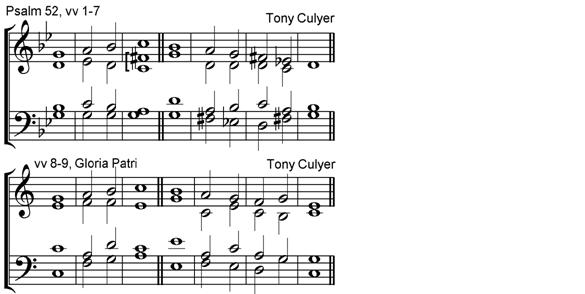
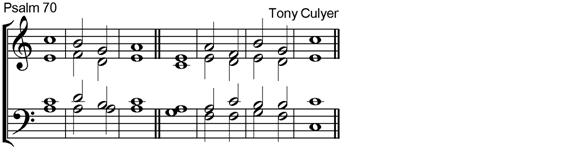
DOUBLE

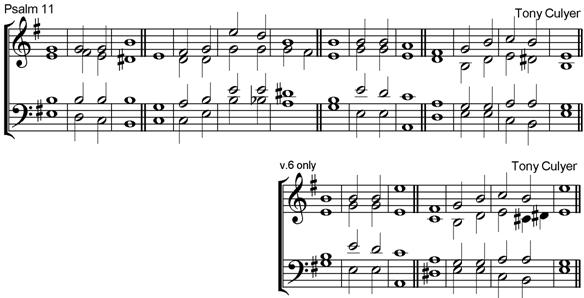
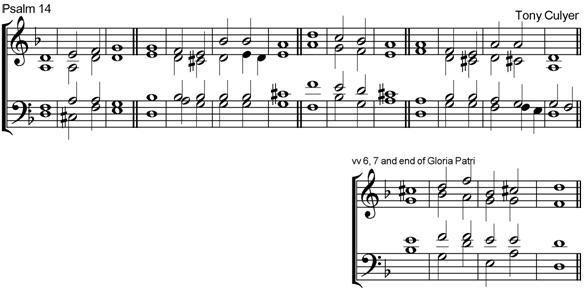
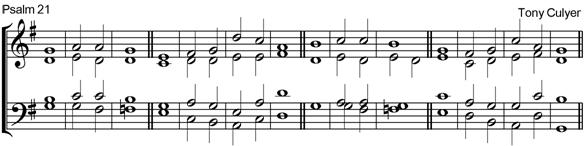
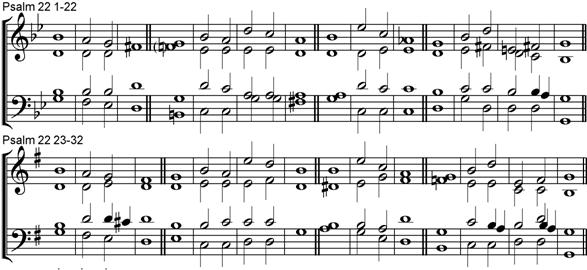
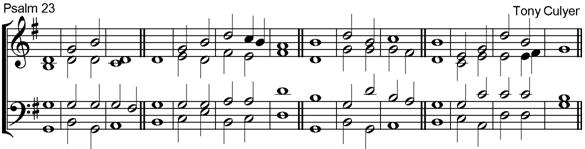
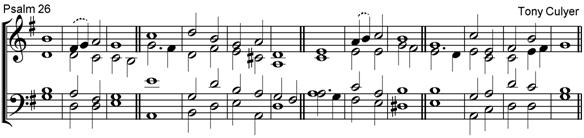
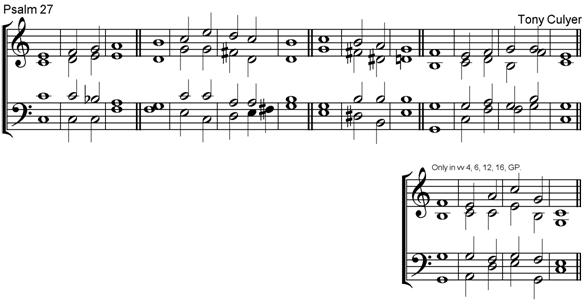
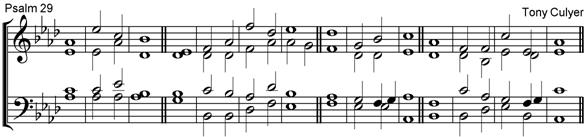
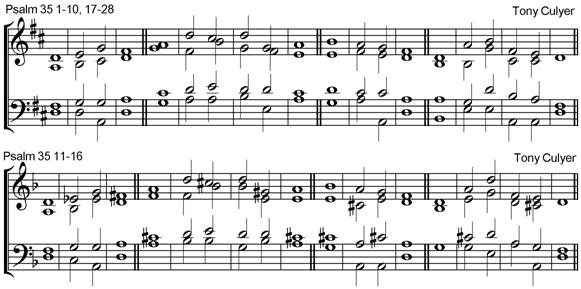
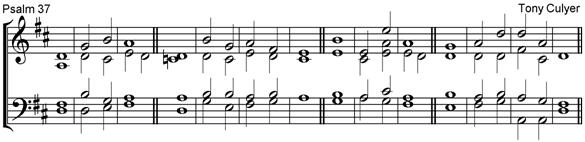
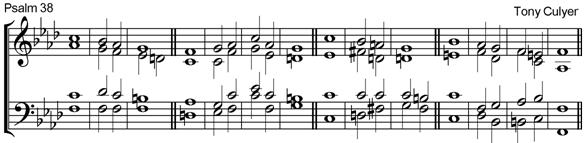


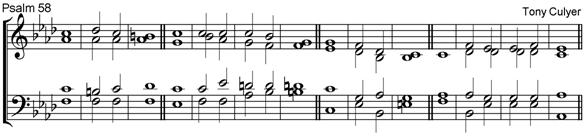
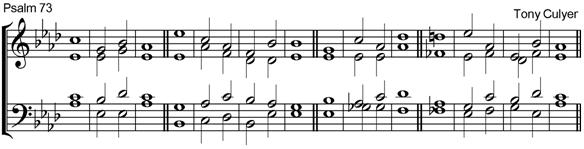

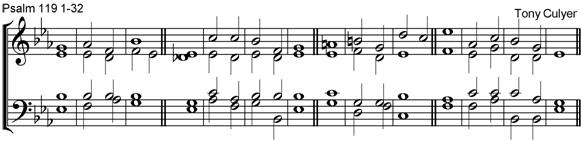
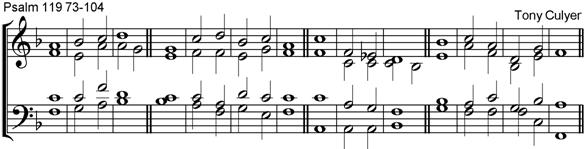

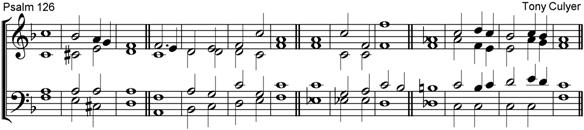
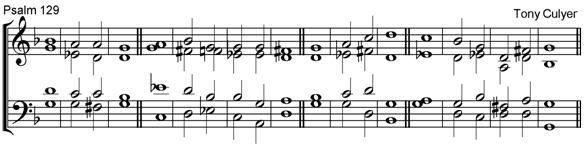
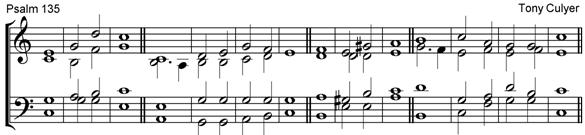
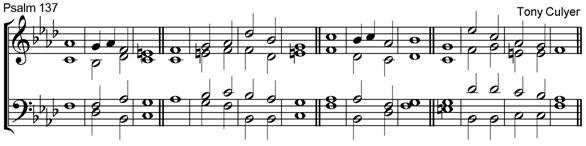
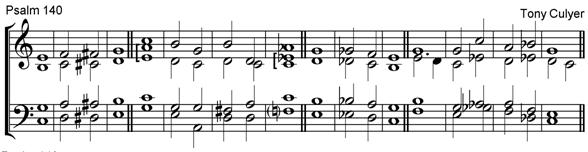




TRIPLE
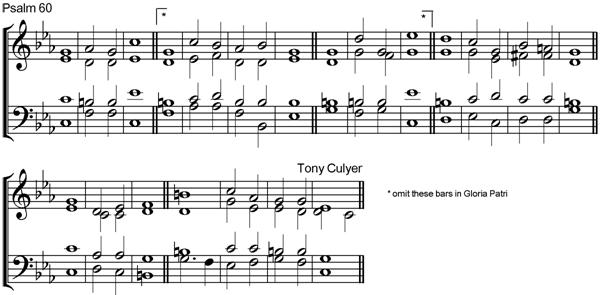
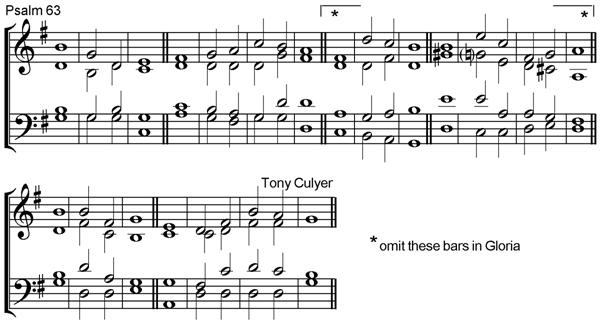
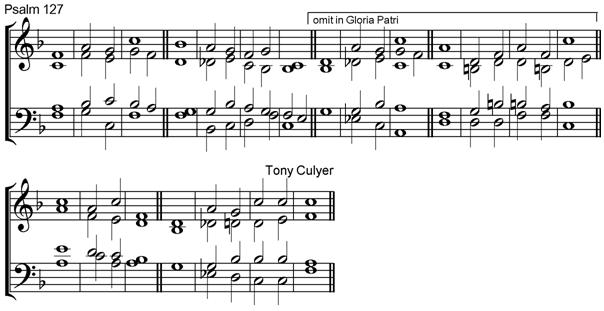
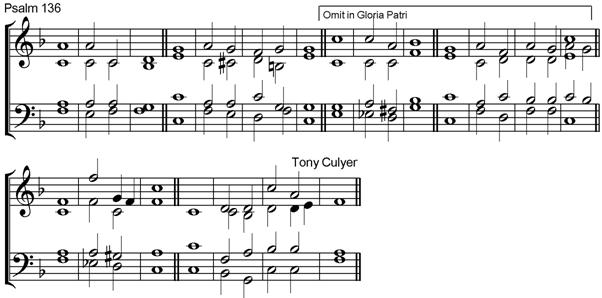
QUADRUPLE
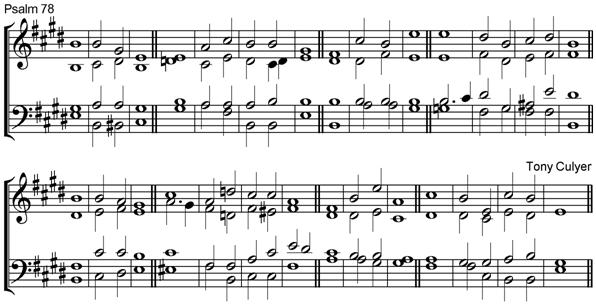

Other pieces
We pray thee, heavenly Father
(homage to John Bacchus Dykes)
Music:Tony Culyer

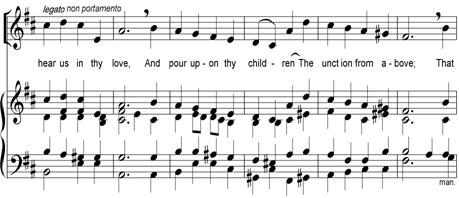
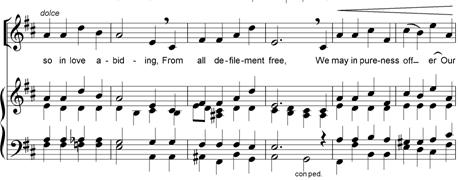
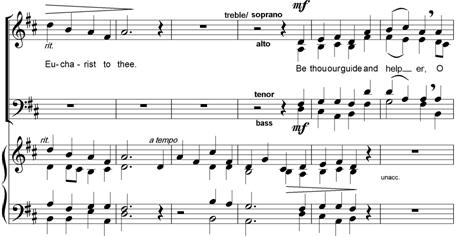
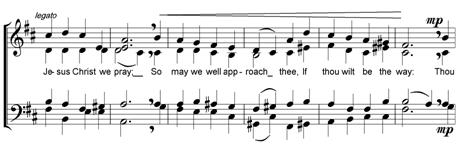
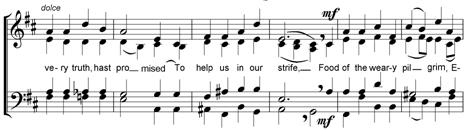
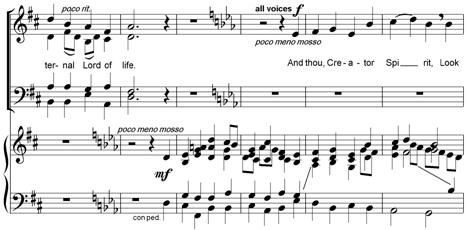
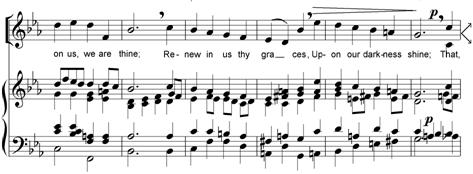

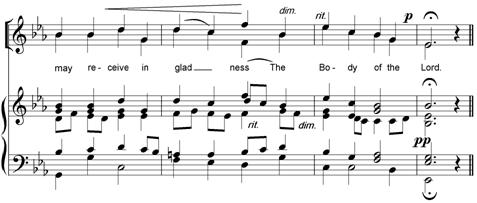
JACOBS LADDER
An Eastertide Carol
Words 18th
Century English Folk Music:
Tony Culyer

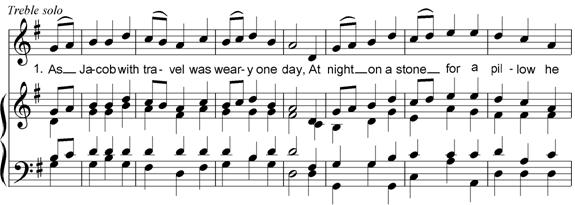
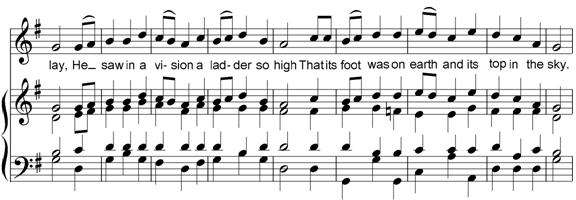
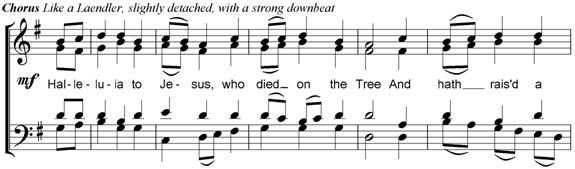
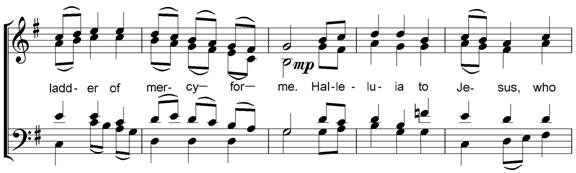
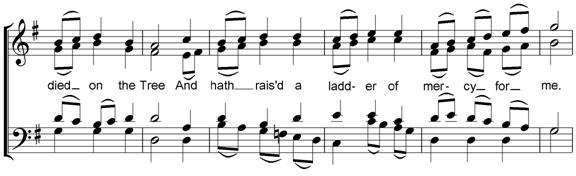

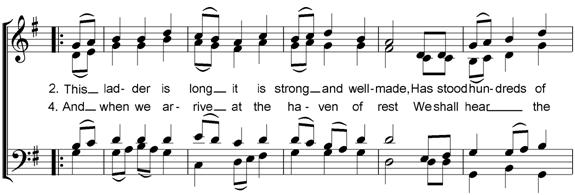
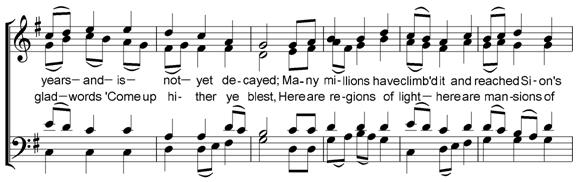
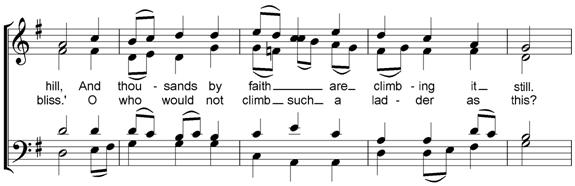
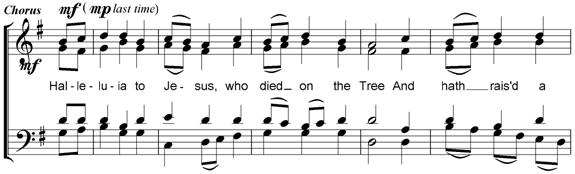
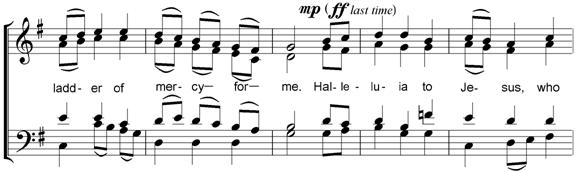
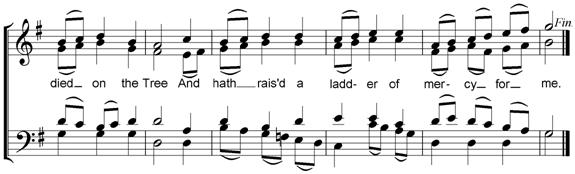

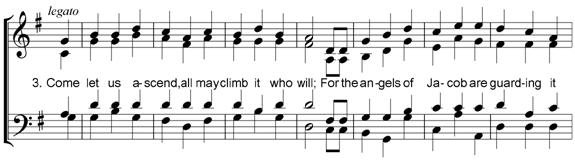
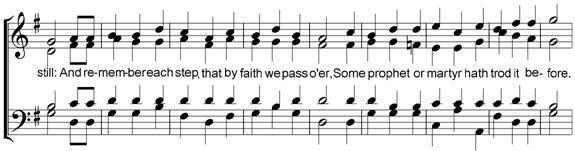
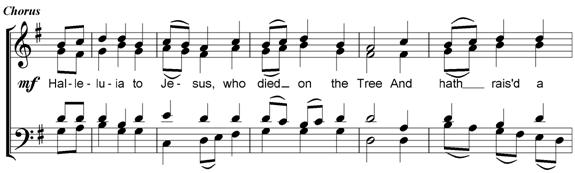
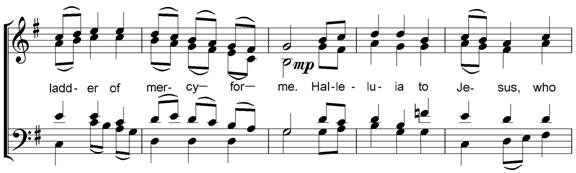
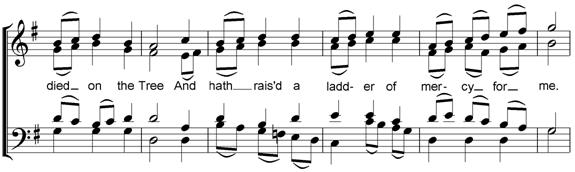

As up the wood I
took my way
Words: Selwyn Image
(1849-1930) Music: Tony
Culyer

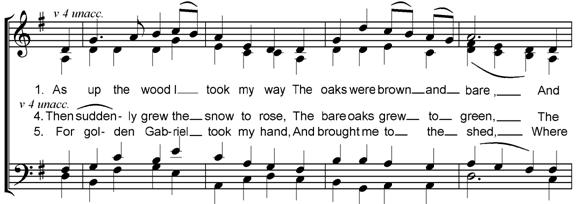
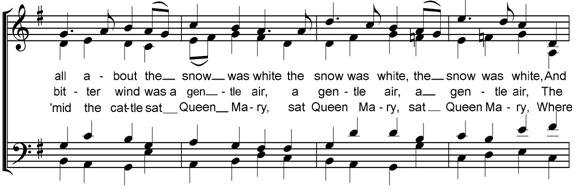
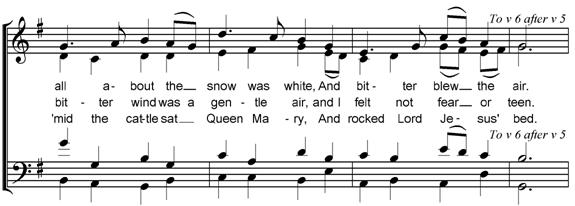

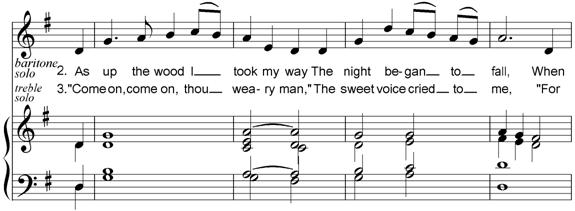
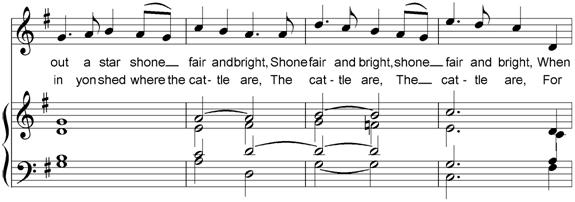
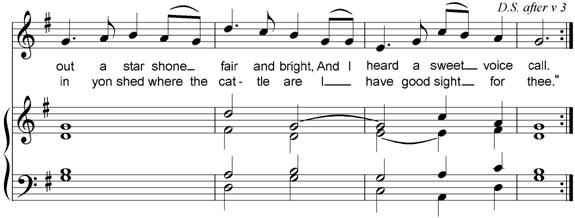

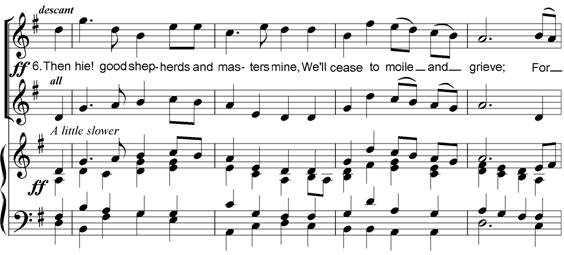
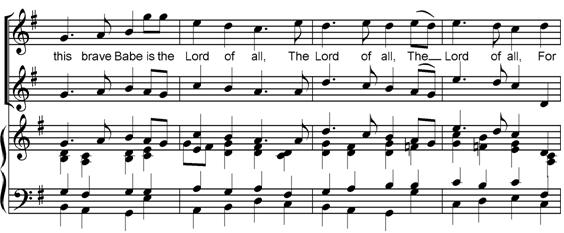
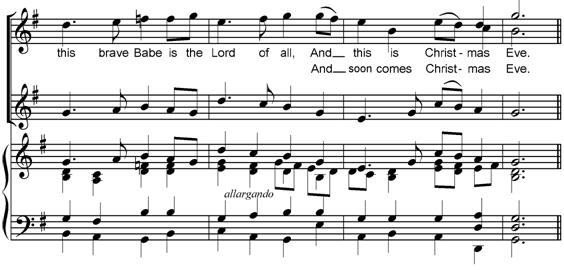
 Return
to index
Return
to index
Hymn Tunes

To 'How shall
we sing salvation's song' by Timothy Dudley-Smith.
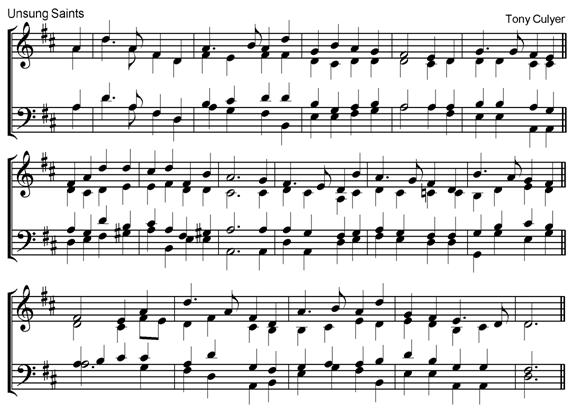
To: We sing for all
the unsung saints, by CARL P. DAW Jr

To: O Christian, love
you sister and your brother! By John Greenleaf Whittier
(1807-1892) (alt.)
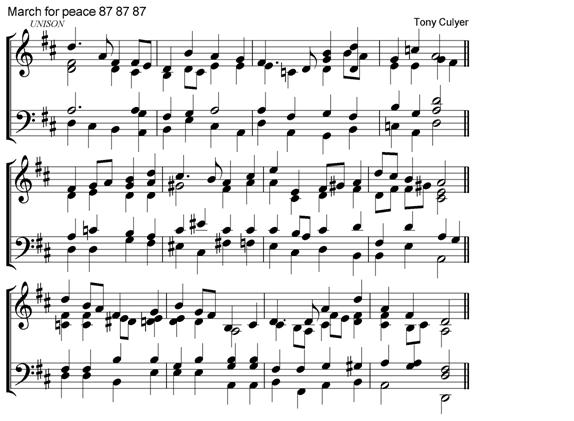
To: GOD of freedom,
God of justice, by Shirley Erena Murray (b. 1931)

To: Bless
the Lord, created things, by Judy Davies
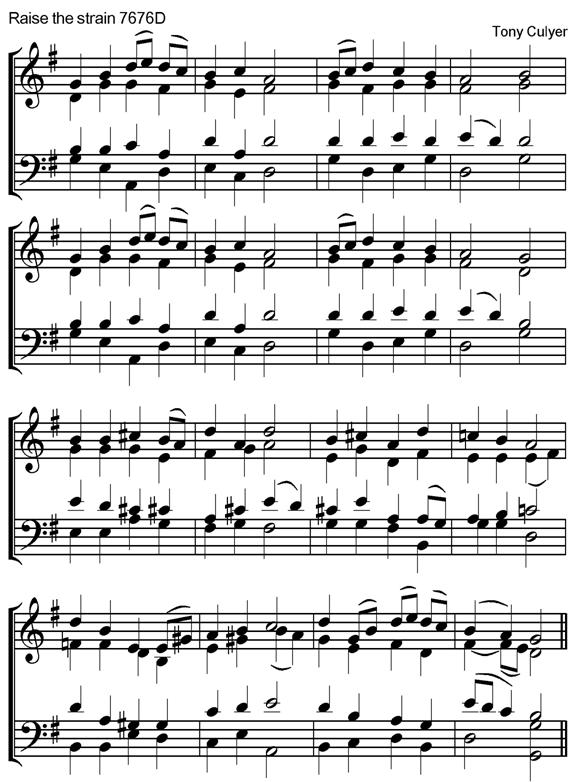
To: Come, ye
faithful, raise the strain of triumphant gladness! By St
John of Damascus
(d. c. 754); (trans. J M Neale 1818-1866)
 Return
to index
Return
to index
Royal School of Church Music
The website of
the RSCM is http://www.rscm.com/. As a
trustee, member of Council and chair of the Voluntary Forum for Chairs, I am happy to receive representations from members and pass
them on the appropriate people. I can be got at by e-mail (tonyandsiegi@btinternet.com). On
matters Canadian, the website is http://www.rscm.com/international/canada.php
and again I am happy as a director on the RSCM (Canada) Board to receive and pass
on representations. My home telephone numbers are (UK)
01759 307177 and (Canada)
416 369 9973.
 Return
to index
Return
to index
CV
Current articles
Journal of Health Economics
Anglican Chants
Other Pieces
Hymn Tunes
Royal School of Church Music

![Text Box: PET: A practical equity tool for HTA decision makers
Guiding Questions:
1 Are we concerned with fairness related to equality or to fair inequality?
[Equality (or inequality) of what? Need, deservingness, responsibility, capacity to benefit (or be harmed), degree of incapacity or current health state, history of past health or ill-health, prognosis with and without the intervention; health outcome -- quality of life; and dependents (care-giving responsibilities)? Do we need quantitative information on any aspect? If there is any inequality of treatment or outcome, for example, by giving some groups a priority status, is it an acceptable inequality? What is the case for it? Is there any evidence base?]
2 Have all possible and relevant aspects of equity been taken into account?
[Should the focus of equity relate to health care inputs or costs, to processes or to outcomes? Might there be unintended consequences of an intervention that raise equity issues? Should the focus be disease or should some other basis for differentiating individuals and subgroups be used? Have equity aspects of the likely ways in which the interventions will be delivered been addressed? Have the Boards (or equivalent) equity requirements been met? Is there any evidence base?]
3 Have legally required factors been addressed?
[Have the relevant local legal obligations concerning age, gender, disability, ethnicity, race, nationality, language, sexual orientation, etc. been considered? Are there any legislative requirements concerning institutionalized, implicit or indirect discrimination?]
4 Are there any general principles of equity that ought to be taken into account?
[Have a set of guiding principles or axioms been established concerning what constitutes equality (or fair inequalities)? If so are they applicable in the current context? Is it possible to derive specific ways of proceeding from the general guidance? Are there any precedents from earlier decisions that we could draw upon?]
5 Are there any inequities embedded in our methods of analysis?
[Are possible inequities built into our concepts (such as omitted dimensions of outcome or cost), have there been biasing framing effects in experimental data, is there possible unfairness inherent in the intervention (such as a threat to some individuals autonomy)? Are the standard weights attached to gains and losses affecting different people (usually but not necessarily, unity) suitable in the current context? Do the empirical measures of inequity (if any) weight distance from the average in an acceptable way? Are there any indirect consequences of the intervention that may raise equity concerns?]
6 Is there any possibility of institutional bias?
[Do any of the following cause particular costs or benefits to be omitted or distorted: our parent organization, the culture of the manufacturers of the interventions, the culture of specific patient advocacy groups, the culture of the HTA experts and their institutions, provider institutions likely to deliver the intervention, workplaces?]
side one
© Anthony J Culyer and Yvonne Bombard 2011](welcome_files/image007.gif)
![Text Box: 7 Is there any possibility of implicit unfair stereotyping?
[Are we using definitions and concepts that inherently exclude or prejudice anyone? Do any aspects of the effects of the intervention have differential impact on individuals, or make untested assumptions about what does and does not matter, or stigmatize? Have assumptions about what matters been tested by consulting those affected? Are there people who might be affected but whose interests have not been taken into account?]
8 Could the current context and circumstances lead to inequity?
[Do any of the following circumstances affect the distribution of negative and positive consequences: geography, demographics (age, sex, ethnicity, socio-economic status), location of delivery of care (such as home or institution), education, language, religion, sexual orientation, or multiple deprivation? Are measures developed for one culture being appropriately applied in another (such as methods used in a high-income country being applied in a low-income country, or western values being applied in an aboriginal or first nations context?]
9 Are our HTA processes fair?
[Has the scoping of the HTA caused a bias in the processes through which information about equity has been gathered or considered? Is our procedure devoid of implicitly biasing elements such as the exclusion of relevant consultation groups? Have the appropriate stakeholders been included in the HTA process (including patients and members of the public)? Is anyone likely to have felt excluded?]
10 Have hidden opportunity costs been neglected?
[Has due regard been given to the interests of the anonymous clients of the health care system who are not the direct beneficiaries of the technologies being considered but from whom resources will be diverted as a consequence of the implementation of the recommendation of this HTA? Do those most likely to be affected in this way have distinctive characteristics suggesting that differential weights ought to be attached to the impacts on them? Are there any empirical estimates of any such relevant effects?]
11 Are the processes of delivery of the technologies equitable?
[Are there processes in the delivery of care, apart from those embedded in institutions, that discriminate unfairly? Are any of the likely delivery processes prejudicial to, demeaning of or embarrassing for some clients relative to others? Is there a middle class bias favouring those with skills at dealing with receptionists, bureaucrats, professionals and other unfamiliar groups?]
12 Are there any special claims that should be addressed?
[Are there interests such as people with needs that are not being heard? Do children, people near death require special consideration? Are their claims ethically significant? Can any claims that might carry weight bear empirical testing for veracity and size?]
13 Do cumulative effects matter?
[Has a holistic perspective been taken of people, or merely separate individual aspects? Have historical disadvantages been considered, especially multiple ones? Are there any other respects in which the cumulative experience or the combination of experiences of those affected may be of equitable concern?]
Side two
© Anthony J Culyer and Yvonne Bombard 2011](welcome_files/image025.gif)